health
The Truth About Mental Health and Why It’s Important to Talk About It

Mental health is a topic that has been shrouded in stigma and silence for far too long. It’s time we start talking about it openly and honestly. The truth is, mental health affects us all – whether we realize it or not. From anxiety to depression, from bipolar disorder to schizophrenia, these conditions can have a profound impact on our lives and the lives of those around us. In this blog post, we’ll delve into why it’s so important to talk about mental health, and how doing so can benefit both individuals and society as a whole. So let’s break down the barriers of shame and ignorance, and start having an open dialogue about this crucial aspect of our well-being!
Mental Health is Real
Mental health is real. It’s a condition that affects millions of people in the United States, and it can be really tough to cope with. That’s why it’s so important to talk about mental health and get help if you need it.
There are a lot of different ways to deal with mental health problems, and there’s no single right way to fix them. You may want to talk to your doctor or therapist about what kind of help you need. Or you could try some self-help techniques, like journaling or meditation.
Whatever you do, don’t keep your mental health problems bottled up. They’ll only get worse if you don’t talk about them and get the support that you need.
Mental Health is Vital
Mental health is vital. Too often, we ignore or avoid talking about mental health because it’s seen as a taboo topic. But mental health is just as important as physical health and should be treated with the same respect.
Mental health affects everyone in different ways, but it can share some common symptoms. These symptoms can include mood swings, an inability to concentrate, feelings of isolation or loneliness, and thoughts of suicide.
If you think you may have mental health issues, don’t wait to get help. There are many resources available to you, and talking about your problems is the best way to get them resolved.
Mental Health is Treatable
What is mental health? Mental health is a state of well-being, where an individual feels accepted and cared for. It’s not just about feeling happy – mental health can include feelings of stress, anxiety, depression, loneliness, sadness, and anger. But it’s not just about your head – mental health also includes your body and emotions.
How do you know if you have mental health problems? You could have symptoms for years without knowing what they are called or what to do about them. Symptoms can include: feeling stressed or anxious most of the time
feeling sad or suicidal
having problems with sleep or concentration
having trouble making decisions
having strong negative thoughts (called “rumination”) For some people, the symptoms might be mild and go away on their own. For others, the symptoms might be more serious and need professional help. There is no one way to look or feel mentally healthy – everyone experiences mental health differently.
The Signs and Symptoms of Mental Illness
Mental illness is a condition that affects your thinking, mood, and behavior. It can make you feel sad, anxious, or stressed. Mental illnesses can also lead to problems with your family and friends, such as problems at work or school.
How to Talk to Your Child About Mental Health
We all know that there is something wrong with our children when they exhibit signs of mental health issues. But what do we do? How can we get our kids to open up and talk to us about what’s going on inside their heads?
There’s no one answer to this question, as the best way to approach talking to your child about mental health will vary based on their age, development, and personal circumstances. However, some tips on how to talk to your child about mental health include:
-Start early: The earlier you start discussing mental health with your child, the better. Let them know that you’re curious about them and want to help them feel comfortable talking about anything that’s troubling them. This also gives you a chance to build a relationship with them where they feel comfortable opening up to you in the future should they need it.
-Be supportive: It’s important not to push or force your child into talking about mental health issues if they don’t want to. Instead, be understanding and supportive of their decisions. Let them know that you’re there for them, regardless of what happens during conversations about mental health.
-Encourage communication: One of the most important things you can do as a parent is encourage open communication between your child and therapist/mental health professionals. If your child feels comfortable communicating with someone outside of family members or close friends, they are more likely to be more candid when talking about their feelings and struggles with mental health
How to Talk to Your Partner About Mental Health
Mental health is a topic that can be difficult to talk about with anyone, but it’s especially hard to talk about with your partner. It can be scary to open up about how you’re feeling, and your partner may not know what to say or do if they feel uncomfortable talking about mental health. But communicating well about mental health is important for both of your long-term happiness.
Here are some tips on how to talk to your partner about mental health:
1. start by acknowledging that there is something going on. Mental health isn’t always easy to spot, so it can be helpful to start by acknowledges that something is definitely wrong. If you catch your partner slipping into a depressive state for example, try not to judge them or ask them why they aren’t feeling well right now. Just reassure them that you love them and want the best for them, and listen attentively as they tell you everything that’s troubling them.
2. encourage communication rather than avoidance. One of the biggest things you can do in order to help your partner deal with their mental health issues is encourage open communication between the two of you. This means being willing to talk about anything and everything, even if it makes you feel uncomfortable at first. By being open and communicative, you will both be able to get better understanding of each other’s experiences which could lead to improved relationships overall.
3. don’t force conversations about mental
Business
Root Canal Treatment in Lahore: Expert Care for Your Teeth
Advanced Root Canal Care in Lahore
Root canal problems are common in Lahore due to delayed dental visits and high sugar intake. Root Canal Treatment in Lahore is not just about pain relief; it is about saving your natural tooth with precision and long-term planning.

Why Root Canal Treatment Is Often the Best Option
When the tooth pulp becomes infected, extraction is not always the right answer. Saving the natural tooth helps maintain bite balance and jaw health. Root Canal Treatment in Lahore focuses on removing infection while keeping the original tooth structure intact, which is critical for long-term oral stability.
Signs That Indicate You Need a Root Canal
Many patients ignore early symptoms and visit only when pain becomes severe. Based on clinical experience, the most reliable indicators include:
- Deep, lingering tooth pain
- Sensitivity to hot or cold lasting more than 10 seconds
- Swelling near the affected tooth
- Darkening of the tooth
Early diagnosis allows Root Canal Treatment in Lahore to be completed in fewer visits with better outcomes.
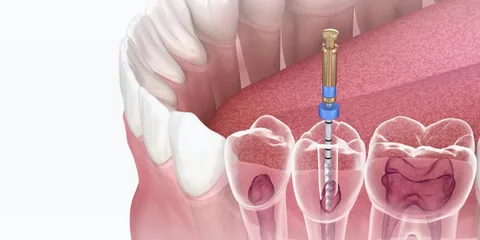
Step-by-Step Root Canal Procedure Explained
This treatment is not a guess-based process. Each step is planned carefully to ensure success.
- Digital imaging to locate infected canals
- Local anesthesia for pain-free treatment
- Removal of infected pulp using rotary instruments
- Thorough canal disinfection
- Sealing with a biocompatible material
This structured approach makes Root Canal Treatment in Lahore predictable and safe.
Expertise Built on 23 Years of Dental Practice
Experience matters in endodontic care. Over 23 years, complex root anatomies, retreatment cases, and failed past procedures have been successfully managed. This level of exposure allows better judgment during Root Canal Treatment in Lahore, especially in molars with curved or hidden canals.
Technology That Improves Treatment Success
Modern dentistry is technology-driven. Advanced clinics use:
- Rotary endodontic systems
- Apex locators for accurate canal length
- Digital radiography with minimal radiation
- Magnification tools for precision
These tools significantly increase the success rate of Root Canal Treatment in Lahore.
Pain Management and Patient Comfort
Many patients fear pain due to outdated myths. In reality, the procedure is more comfortable than tooth extraction. Proper anesthesia, gentle techniques, and post-care planning ensure Root Canal Treatment in Lahore is a smooth experience even for anxious patients.
Post-Treatment Care for Long-Term Results
A root canal-treated tooth needs protection to last many years. After the procedure:
- A dental crown is usually recommended
- Oral hygiene must be maintained
- Regular follow-ups help detect early issues
With correct care, Root Canal Treatment in Lahore can preserve a tooth for decades.
Cost Factors and Treatment Planning
Costs vary depending on tooth type and infection severity. Molars require more time and expertise. Transparent consultation ensures patients understand the value behind Root Canal Treatment in Lahore, rather than focusing only on price.
Why Patients Trust Ideal Smile Dentistry
At Ideal Smile Dentistry, treatment decisions are based on clinical evidence, not shortcuts. Patients benefit from ethical diagnosis, advanced tools, and long-term planning rather than temporary fixes. This approach has built trust across Lahore’s dental community.
Why Experience Matters in Root Canal Dentistry
Dentistry is not just technical; it is judgment-based. After 23 years in dental surgery and clinical practice, patterns become clear. Knowing when to treat, retreat, or refer is what ensures patient safety and success. An experienced dentist can quickly assess complex cases, anticipate potential complications, and tailor treatments effectively.
This level of experience cannot be replaced by shortcuts or rushed procedures. Each patient’s unique anatomy and history warrant careful consideration and personalized care, which only comes from years of practicing and refining one’s skills.
Choosing the Right Dental Clinic in Lahore
Patients should look for:
- Experienced dental surgeons
- Modern diagnostic tools
- Clear treatment explanations
- Transparent pricing
- Long-term follow-up care
At Ideal Smile Dentistry, patient trust is built through experience, not marketing promises.
Frequently Asked Questions About Root Canal Treatment in Lahore
Is root canal treatment safe?
Yes, it is a routine and scientifically proven dental procedure with a high success rate.
How many visits are required?
Most cases are completed in one or two visits, depending on infection severity.
Will I need a crown after treatment?
In most cases, yes. A crown protects the treated tooth from fracture.
Can a failed root canal be retreated?
Yes, retreatment is possible and often successful with proper expertise.
Internal Resources for Patients
For related services, patients can explore:
- Tooth pain diagnosis guide
- Dental crowns and caps services
- Emergency dental care in Lahore
These resources help patients understand treatment options beyond Root Canal Treatment in Lahore.
Summary
Root canal treatment saves natural teeth, relieves pain, and restores oral health. With 23 years of surgical experience, advanced tools, and ethical care, patients in Lahore can expect reliable, long-lasting results when the procedure is done correctly.
Care
Natural Headache Relief: The Massage Therapy Solution

Headaches disrupt everything. They break your focus at work. Even ruin your sleep. They strain time with family and friends. Many people immediately choose pain medicine. It feels quick and easy. However, medicine often just masks the pain. It rarely solves the underlying problem. The pain usually returns.
Maybe you want a different solution. You might seek an approach that helps your body heal. Massage therapy is now a powerful option. It specifically targets tight muscles and stress patterns. These issues commonly cause headaches. Correctly applied, massage can reduce your pain naturally.
This guide explains exactly how headache massage works. Learn why it offers a reliable path to long-term relief.

How Massage Reduces Pain Naturally
Massage supports your body’s own healing process. It does not just cover symptoms. Let’s explore the key mechanisms.
First, it releases muscle tension.
Tight neck and shoulder muscles often trigger pain. Desk jobs and phone use strain these areas. This tension presses directly on nerves. Then, pain signals shoot to your head. Massage applies steady, deliberate pressure. It loosens these specific muscles. Reduced tension decreases nerve pressure. You will feel less stiffness. Fewer pain signals will fire. Regular sessions keep muscles relaxed longer. This directly prevents many headaches from starting.
Next, it improves blood circulation.
Tight muscles restrict healthy blood flow. Your head and neck then get less oxygen. Poor circulation can intensify headache pain. Massage gently manipulates soft tissue. This action encourages better blood flow. Improved circulation helps tissues heal and recover. Many people feel immediate warmth and ease in their neck afterward. Better blood flow can lower both the intensity and duration of headaches over time.
Additionally, it calms your nervous system.
Stress is a major headache trigger. It keeps your body in a tense “fight or flight” state. Your breathing becomes shallow. Muscles tighten unconsciously. This buildup often explodes into a headache. Massage triggers your relaxation response. It shifts your nervous system into a “rest and digest” state. Your muscles unwind. Your breathing deepens. This breaks the stress-pain cycle. You gain a tool to manage tension before it becomes a headache.
Also, it corrects posture problems
Your posture directly impacts headaches. Forward head posture (like looking at a screen) strains your neck muscles. This strain builds slowly but surely. It creates perfect conditions for chronic pain. Massage targets these overworked postural muscles. It releases the tight areas that pull your skeleton out of line. As your posture improves, mechanical strain on your neck decreases. This leads to fewer headaches and more daily comfort.
Critically, it offers sustainable relief
Medicine has its place for acute crises. However, long-term reliance poses problems. These include side effects and medication-overuse headaches. Massage provides a different, sustainable path. It builds body awareness and supports natural function. You can use it regularly without negative consequences. Many people combine it with stretching and stress management. This creates a holistic, proactive routine.
What to Expect from a Session
A professional headache massage is highly targeted. It is not a general relaxation session. First, your therapist will ask detailed questions. They will want to understand your pain patterns, daily activities, and medical history. This assessment guides their hands-on work.
The treatment typically focuses on your upper body. Key areas include your suboccipital muscles (skull base), neck, shoulders, and upper back. Therapists use specific techniques like myofascial release and trigger point therapy. They apply precise pressure to release muscle “knots” and tight fascia. The pressure is firm but should not cause sharp pain. Communication with your therapist is essential. Always tell them if the pressure is too much.
A session usually lasts between 30 to 60 minutes. Afterwards, you might feel deeply relaxed. Some mild soreness is possible, similar to post-exercise feeling. This normally fades within a day. Drink plenty of water. This helps flush metabolic waste released from your muscles.
Building a Long-Term Strategy
For chronic headaches, consistency matters. One massage might offer temporary relief. A series of sessions creates lasting change. It retrains tense muscles and resets poor posture. Many people start with weekly sessions. They then move to bi-weekly or monthly maintenance.
Your therapist can also give you tools for home. They may teach you simple neck stretches or self-massage techniques. They might advise on desk ergonomics or stress-reduction practices. This empowers you to take control between appointments.
Making the Choice for Your Health
Headaches can control your life, but you have options. If your pain stems from tension, stress, or posture, massage addresses these roots directly. It is a practical, drug-free method to reduce pain frequency and severity.
Choose a qualified professional. Look for a licensed massage therapist experienced in clinical or therapeutic work. Be clear about your headache history and goals.
Commit to a plan. Partner with your therapist. Give the process a few sessions to work. Combine hands-on care with the lifestyle changes they recommend.
Ultimately, this approach is about more than pain relief. It is about reclaiming your focus, your sleep, and your daily joy. It is an investment in a life with fewer interruptions and more comfort. Take the step toward lasting relief. Your body—and your calm, clear head—will thank you.
Care
Why CBD Intimacy Oil Is the Must-Try Product of the Year

Connection begins long before any physical moment. It starts with how relaxed you feel in your body and how present you are with yourself. That is why more people are turning toward plant-based wellness to support intimacy in a more natural way.
Products inspired by healing spirits herbs focus on calming the nervous system, supporting sensitivity, and creating an environment where closeness feels easy rather than forced. This shift reflects a deeper desire for comfort, trust, and genuine connection.
As conversations around wellness grow more open, CBD intimacy oil has moved into the spotlight. Many people actively search for CBD intimacy oil for sale because it offers a gentle, supportive option rather than an aggressive solution. Instead of masking discomfort or pushing the body, it works with natural rhythms to encourage relaxation and ease. That alone makes a noticeable difference in how intimate moments unfold.

What makes CBD intimacy oil different from traditional products
Unlike conventional lubricants or enhancement products, CBD intimacy oil supports the body on multiple levels. It does not rely on numbing agents or synthetic stimulants. Instead, it focuses on comfort, circulation, and calm.
Key qualities that set it apart include:
- Plant-based ingredients that feel gentle on sensitive skin
- CBD compounds are known for their soothing and relaxing effects
- Oils that nourish the skin rather than dry it out
- A focus on comfort instead of performance pressure
These qualities allow intimacy to feel more organic and less goal-driven.
CBD works with the body’s endocannabinoid system, which plays a role in regulating stress, sensation, and balance. When the body feels safe and relaxed, it naturally becomes more receptive. This is why many people report improved comfort and awareness when using CBD-infused products during intimate moments.
The emotional side of physical comfort
Physical ease and emotional connection often move together. When the body holds tension, the mind follows. CBD intimacy oil helps reduce that tension, which allows people to stay present rather than distracted.
Reduced discomfort leads to:
- Less anxiety around intimacy
- Greater confidence in one’s body
- Improved communication with a partner
- A slower, more mindful pace
These changes may feel subtle at first, but they build over time. Intimacy becomes less about effort and more about shared experience.
Wellness routines outside the bedroom also play a role. Many people who explore CBD intimacy oil already value calming rituals throughout the day. Practices like stretching, quiet evenings, or choosing to buy herbal teas and tisanes help create a relaxed baseline. When the nervous system feels supported daily, intimate moments feel more natural and enjoyable.
How to use CBD intimacy oil with intention
Using CBD intimacy oil works best when you slow down and stay attentive. Rushing defeats the purpose. Treat the oil as part of the experience, not a tool to get past discomfort as quickly as possible.
Helpful guidelines include:
- Start with a small amount and add more only if needed
- Warm the oil between your hands before applying
- Use slow, mindful touch rather than quick movements
- Communicate openly about comfort and preferences
This approach turns the application into a shared ritual instead of a mechanical step.
Many couples find that intention matters as much as the product itself. Setting aside distractions, lowering lights, or playing calming music helps reinforce the sense of safety and presence. CBD intimacy oil simply supports what the environment already encourages.
Choosing quality and transparency
Not all CBD products meet the same standards. Ingredient quality, sourcing, and formulation matter, especially for intimate use. Reputable wellness brands focus on clean ingredients and clear labeling.
When choosing a product, look for:
- Third-party testing for purity and potency
- Simple ingredient lists without harsh additives
- Clear guidance on usage and storage
- Brands that prioritize education, not hype
This level of transparency builds trust and ensures the product aligns with a holistic approach to wellness.
Many people prefer shopping through a trusted apothecary in Denver or similar wellness-focused retailer because these spaces emphasize quality, ethics, and customer education. This makes it easier to choose products that truly support well-being rather than chase trends.
Why CBD intimacy oil fits modern wellness values
Today’s wellness culture values balance, consent, and self-awareness. CBD intimacy oil fits naturally into this mindset. It does not promise instant transformation. Instead, it supports comfort, communication, and connection over time.
This product resonates because:
- It respects the body’s natural responses
- It encourages slower, more mindful experiences
- It aligns with plant-based and holistic lifestyles
- It supports intimacy without pressure or expectations
These qualities reflect a broader shift away from quick fixes and toward sustainable well-being.
CBD intimacy oil has earned its place as a must-try product because it supports both body and mind. Easing tension, improving comfort, and encouraging presence help intimacy feel more natural and connected. When paired with thoughtful self-care and honest communication, it becomes part of a wider wellness practice that values depth over speed and connection over performance.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom