health
Eating for a Healthy Mind: The Role of Nutrition in Mental Wellness

Do you ever wonder how the food you eat affects your mental health? It’s no secret that a balanced diet is essential for maintaining physical wellness, but did you know that nutrition also plays a significant role in our mental well-being? From improving cognitive function to reducing symptoms of depression and anxiety, the right nutrients can help us maintain a healthy mind. In this blog post, we’ll explore the intricate relationship between what we eat and how it impacts our brain function. So grab a snack (preferably something nutritious!) and let’s dive into the fascinating world of eating for a healthy mind.
What is Nutrition and Mental Health?
Mental health is a state of mind, which can be affected by many factors such as stress, anxiety, and depression. Diet is one important factor in maintaining mental health, as it plays a role in regulating mood and cognitive function. Nutrition is the food we eat and how it impacts our body and mind.
There are many different types of mental illnesses, but all share some common features. Mental illness can interfere with daily functioning, cause feelings of sadness, loneliness, and hopelessness, and impact relationships. It can also make it difficult to obtain or maintain employment or maintain healthy habits.
There is no one-size-fits-all approach to treating mental illness, but there are several key things that nutritionists believe play an important role in promoting good mental health. Nutritional deficiencies can lead to imbalances in neurotransmitters (brain chemicals) that can contribute to symptoms of depression or anxiety. A well-balanced diet that includes whole grains, fruits, vegetables, lean protein sources, Omega-3 fatty acids,, magnesium, antioxidants ,and phytonutrients can help restore balance within the body and support positive mental health outcomes.
In addition to diet ,it’s important to consider lifestyle factors such as exercise and socializing when trying to improve mental health. Exercise has been shown to boost mood and decrease symptoms of depression ,while socializing has been linked with reducing feelings of isolation . Ensuring adequate sleep is also essential for overall well-being; people who struggle
The Role of Nutrition in Mental Health
Mental health is a state of mind characterized by feelings of well-being, happiness, and calmness. It can be improved by eating a balanced diet that includes sufficient amounts of essential vitamins and minerals.
The brain is mainly composed of water, proteins, carbohydrates, and fats. Carbohydrates are the most important source of energy for the brain. The body needs glucose to produce energy and to run the central nervous system. Glucose is found in foods such as fruits, vegetables, grains, beans, and legumes. A good mental health diet should include plenty of these healthy carbs.
Fats are also important for the brain. They help to keep cells hydrated and provide them with Essential Fatty Acids (EFAs), which are important for cognitive function and mood regulation. Dietary fats can be classified into saturated or unsaturated fats. Saturated fats are unhealthy because they increase bad cholesterol levels in the blood. Unsaturated fats have been linked with lower rates of heart disease and some types of cancer.
A good mental health diet should also include plenty of fiber. Fiber helps regulate blood sugar levels and keeps you feeling full longer so you don’t overeat.”
The Types of Mental Illness
Mental illness can be caused by a variety of factors, including genetics, environmental exposures, and lifestyle choices. Mental health professionals often use the terms “mental disorder” and “mental health condition” to refer to different types of conditions that affect a person’s mood, thinking, or behavior.
There are nine officially recognized mental disorders in the United States: anxiety disorders (including panic disorder and generalized anxiety disorder), mood disorders (depression and bipolar disorder), substance use disorders (alcohol abuse and addiction), eating disorders (anorexia nervosa and bulimia nervosa), schizophrenia and schizoaffective disorder, ADHD (attention-deficit/hyperactivity disorder), autism spectrum disorder. In addition to these nine mental disorders, there are dozens of other mental health conditions that do not fit neatly into one of those categories.
There is no single cause for mental illness, but many factors can contribute. Some people with mental illnesses may have a genetic vulnerability that leads to development of the condition. Environmental exposures – such as stressors at home or at school – can also play a role in the development of mental illness. Lifestyle choices such as smoking cigarettes or using alcohol can also increase the risk for developing certain mental illnesses.
The Role of Nutrition in Mood Regulation
The relationship between diet and mental health is complex and still largely unknown. There is some evidence that a diet high in fruits, vegetables, nuts, and whole grains may be associated with improved mental health. It is also known that dietary deficiencies can cause mood disorders.
While the exact role of nutrition in mood regulation remains to be fully understood, it is clear that maintaining a healthy balance of nutrients can play an important role in overall brain health and well-being. In particular, vitamin B6 (pyridoxine), magnesium, omega-3 fatty acids (EPA and DHA), and chromium have all been linked with better mood regulation.
If you are looking to improve your mental well-being, it is important to consider what foods are providing you with the nutrients you need for optimal brain function. Talk to your doctor about your individual dietary needs and how best to ensure they are being met.
The Role of Nutrition in Emotional Well-being
Nutrition is an essential part of a healthy mind and body. Not only does good nutrition help to maintain physical health, it has been shown to play a role in mental well-being as well.
There are several key components to a nutritious diet, including:
Fiber: One of the key nutrients responsible for maintaining good mental health is fiber. Fiber helps to keep your digestion running smoothly and can help to reduce the risk of chronic diseases such as heart disease, cancer, and diabetes. Aim to eat at least 25 grams of fiber each day.
Healthy fats: Healthy fats are important for both your mental and your physical health. They can help you feel fuller longer and support mood stability and cognitive function. Some great sources of healthy fats include olive oil, nuts, seeds, avocado, and fish oils. Aim to consume around 20-30 grams of healthy fats each day.
Complex carbohydrates: Complex carbs are important for providing energy throughout the day. They also have other benefits such as promoting gut health and helping to regulate blood sugar levels. Aim to consume around 45-60 grams of complex carbs each day.
How to Eat for a Healthy Mind
Nutrition is an essential part of brain health and function. Food can provide the building blocks for neurotransmitters, which are chemicals that help relay messages between nerve cells. Eating a balanced and nutritious diet has been shown to improve mental well-being across the board, from memory and concentration to mood and stress levels. Here are five ways nutrition can support mental health:
1) Eat foods that promote cognitive function. Foods high in antioxidants, like berries, green leafy vegetables, and nuts, are packed with nutrients that help protect the brain against damage caused by toxins and inflammation. They also contain phytonutrients, which have anti-inflammatory properties. These nutrients work together to improve neurological function and protect against chronic disease.
2) Include plenty of protein in your diet. Protein is important for neurotransmitter production and helps preserve muscle mass while you’re trying to lose weight or maintain a healthy weight. It also helps keep blood sugar levels stable so you don’t experience those sudden cravings or mood swings associated with eating too much sugar or carbs.Aim for about half your daily caloric intake from protein sources such as lean meats, poultry, seafood, eggs, legumes (beans), yogurt, cheese, and plant proteins like hemp seeds (hemp milk).
3) Eat more fiber-rich foods. Fiber is critical for gut health because it helps regulate blood sugar levels and keeps us feeling full longer after we eat. A high-fiber diet has
Conclusion
As we all know, mental well-being is essential for a productive and happy life. Nutrition has long been recognised as an important factor in maintaining mental wellbeing, and recent studies have shown that there is much more to nutrition than simply filling our stomachs. In fact, the role of nutrition in mental health goes far beyond just providing us with the nutrients our bodies need to function properly – it also plays a role in regulating mood and cognitive function. As we learn more about how diet can play a role in promoting overall mental health, let’s make sure to include good quality foods into our everyday lives not only for their nutritional value but also for their ability to promote relaxation and stress relief.
Care
Prenatal Multivitamin Gummies: A Guide for Expecting Mothers

Pregnancy is a time of great change for expecting mothers. During these nine months, proper nutrition becomes more important than ever, as it supports both the health of the mother and the development of the baby.
While a balanced diet is essential, it can be difficult for many expecting moms to get all the nutrients they need through food alone.
This is where prenatal vitamins, especially prenatal multivitamin gummies, play a critical role. These chewable supplements provide an easy, convenient, and effective way for mothers to ensure they are getting the necessary nutrients.

Why Prenatal Multivitamin Are a Game Changer for Expecting Moms
Prenatal multivitamin gummies offer a number of benefits that make them an appealing option for pregnant women. Not only are they a tasty alternative to traditional pills, but they also provide essential vitamins and minerals that are critical during pregnancy.
1. Convenience and Ease of Consumption
For many women, swallowing large pills can be difficult, particularly during pregnancy when nausea and morning sickness are common. Prenatal multivitamin gummies offer a much more palatable and enjoyable alternative.
With a variety of flavors and the ease of chewing rather than swallowing pills, these gummies help ensure that moms-to-be are more likely to stay consistent with their supplementation.
Additionally, their compact size and convenience make it easy to incorporate into daily routines. Whether at home or on-the-go, prenatal gummies can be taken at any time, ensuring moms don’t miss out on vital nutrients.
2. Rich Source of Essential Nutrients
Prenatal multivitamin gummies are formulated to support the nutritional needs of pregnant women. These gummies typically include vital vitamins and minerals such as:
- Folic Acid: This B-vitamin is one of the most important for a healthy pregnancy. Folic acid helps prevent birth defects of the brain and spine and is essential for fetal development.
- Iron: Pregnant women are at a higher risk of anemia due to increased blood volume. Iron helps support the increased demand for oxygen-carrying red blood cells and aids in preventing iron-deficiency anemia.
- Calcium: This mineral is necessary for the development of the baby’s bones and teeth. It additionally aids in preserving the mother’s bone health throughout pregnancy.
- Vitamin D: Vitamin D supports the immune system and helps the body absorb calcium more efficiently, which is critical for both the mother and the baby.
- Iodine: Iodine is crucial for proper thyroid function and plays a key role in the baby’s brain development.
Many prenatal gummy supplements also include other beneficial nutrients such as Vitamin A, Vitamin C, and Zinc, all of which play a part in immune function, skin health, and overall wellness for both mom and baby.
3. Better Absorption and Less Risk of Stomach Upset
Unlike traditional prenatal pills, which can be tough on a sensitive stomach, prenatal multivitamin gummies are generally easier to digest and less likely to cause stomach upset.
Many pregnant women experience nausea, heartburn, or indigestion, especially during the first trimester. Gummies tend to be gentler on the digestive system, allowing moms to get the essential nutrients without the discomfort associated with pill form.
Moreover, since these vitamins are in a chewable form, they are absorbed more quickly into the bloodstream, leading to faster and potentially more efficient nutrient delivery to both mother and baby.
4. Improved Adherence to Prenatal Supplementation
One of the challenges many expecting mothers face is maintaining consistency with their prenatal supplementation. Studies have shown that when prenatal vitamins are in a more appealing form, like gummies, women are more likely to follow their supplementation schedule.
The tasty flavors make it easier for pregnant women to take their daily dose without forgetting or feeling overwhelmed by the process.
This consistent adherence helps ensure that both the mother and baby receive the required nutrients every day, supporting healthy growth and development throughout the pregnancy.
The Role of Prenatal Multivitamin Gummies in Supporting a Healthy Pregnancy
Prenatal multivitamin gummies play an essential role in filling nutritional gaps that may exist in the diet of an expecting mom. While a well-balanced diet should ideally provide all the necessary nutrients, pregnancy increases a woman’s nutritional requirements.
Often, women experience food aversions or cravings, making it difficult to maintain a balanced diet. These nutritional gaps can be addressed with the help of prenatal multivitamin gummies, ensuring that mom and baby have the vitamins and minerals they need.
Furthermore, supplements like prenatal vitamins have been shown to help reduce the risk of pregnancy complications, including preterm labor and low birth weight.
Consuming the right combination of nutrients during pregnancy also helps optimize fetal development, ensuring babies are born healthy and strong.
How Prenatal Multivitamin Gummies Help With Specific Pregnancy Symptoms
Pregnancy can bring with it a variety of symptoms, some of which can be mitigated with proper supplementation. Prenatal multivitamin gummies, with their specific formulation of vitamins and minerals, are designed to help with the following common pregnancy concerns:
- Morning Sickness: Prenatal gummies are typically easier on the stomach and less likely to induce nausea compared to traditional tablets. Vitamin B6, which is commonly found in these gummies, is known to help reduce nausea, making it a popular remedy for morning sickness.
- Fatigue: The increased iron content in prenatal multivitamin gummies can help combat fatigue caused by low iron levels. Iron is essential for producing red blood cells that carry oxygen to both the mother and baby, helping moms-to-be feel more energized.
- Immune Support: Pregnancy often weakens the immune system, and supplements like Vitamin C and Zinc found in prenatal multivitamins help bolster the immune system. These vitamins support the body in fighting off infections and maintaining overall health during pregnancy.
Are Prenatal Multivitamin Gummies as Effective as Traditional Pills?
Many expecting mothers may wonder whether prenatal gummies are as effective as traditional pill supplements. The answer largely depends on the specific formulation of the product.
While both forms of supplementation are effective, gummies tend to offer a slightly higher level of bioavailability, meaning that the body absorbs them faster and more efficiently.
However, it is important to choose a high-quality prenatal gummy that contains the right balance of nutrients. Not all gummy supplements are created equal, so it’s important to consult with a healthcare provider to ensure the product meets the specific nutritional needs of the mother and baby.
Conclusion
Prenatal multivitamin gummies are an excellent option for expecting mothers seeking a convenient, gentle, and effective way to support their pregnancy health.
With essential vitamins and minerals like folic acid, iron, calcium, and Vitamin D, these gummies provide a vital source of nutrients for both the mother and the developing baby.
They are particularly beneficial for women who may struggle with traditional prenatal pills or those who experience nausea during pregnancy.
By making it easier to stay consistent with supplementation, prenatal multivitamin gummies help ensure that the mother’s nutritional needs are met, supporting healthy fetal development and a smoother pregnancy journey.
For expecting mothers, choosing high-quality prenatal multivitamin gummies can truly make a difference in how they feel and how their pregnancy progresses, providing peace of mind and a healthier start for both mom and baby.
Care
Leukoplakia: Causes, Symptoms, and Treatment for Oral Health

White patches inside the mouth can be worrying, especially when they appear unexpectedly or refuse to go away. Among the most common causes of such patches is a condition known as leukopakia. While it is often harmless, leukoplakia can occasionally signal early signs of more serious problems, making awareness and early detection essential.
Understanding what leukoplakia looks like, why it develops, and how it is treated empowers individuals to take charge of their oral health. This guide walks you through the key facts, symptoms and treatment options, offering clarity and confidence for those who may be noticing unusual changes in their mouth.
What Is Leukopakia?
Leukoplakia refers to thickened white or grey patches that form inside the mouth due to excessive cell growth, often triggered by long-term irritation. These patches may appear on the gums, inner cheeks, tongue, or roof of the mouth. While many cases are harmless, some require monitoring to ensure no further complications develop. Early detection is important because changes can sometimes indicate underlying issues.
Types of leukoplakia:
- Ordinary leukoplakia: Commonly linked to tobacco use and continual irritation.
- Hairy leukoplakia: Associated with viral infections and seen more frequently in individuals with weakened immune systems.
Identifying leukoplakia early helps ensure abnormalities are evaluated promptly and managed before they progress.

What Do Leukoplakia Patches Look Like?
Leukoplakia patches usually appear as uneven, slightly raised areas that feel rough and range in color from white to grey. They cannot be scraped off, which helps distinguish them from conditions like oral thrush. Although generally painless, some people may notice mild sensitivity or irritation, especially when consuming hot or spicy foods. Sudden changes in appearance should be taken seriously.
Warning signs that require urgent evaluation:
- Patches turning red or darkening
- Rapid growth in size
- Increasing discomfort or sensitivity
These changes are often first spotted during brushing or routine dental visits, highlighting the importance of regular check-ups with a dentist or a hygienist in Chichester.
Common Causes & Risk Factors
Leukopakia can be triggered by several factors. Some of the most common include:
Lifestyle-related causes
- Tobacco use: Smoking or chewing tobacco remains the most significant cause, responsible for the majority of diagnosed cases.
- Excessive alcohol consumption: Alcohol irritates the oral tissues and magnifies the effects of smoking when combined.
Irritation-related causes
- Rough or sharp teeth rubbing against the inside of the mouth
- Poorly fitted dentures
- Chronic cheek or tongue biting
Medical and biological factors
- Viral infections such as Epstein–Barr virus
- Weakened immune systems
- Ageing and prolonged exposure to irritants
In some instances, individuals discover leukoplakia when visiting an emergency dentist in Chichester due to pain, bleeding or sudden irritation, even though these signs are not always directly caused by the patches themselves.
Diagnosis: How Professionals Identify Leukoplakia
Diagnosing leukoplakia usually starts with a clinical examination, where a dental professional assesses the affected area, reviews medical history, and asks about habits such as smoking or alcohol use. If a patch persists for more than two weeks, further investigation is required to determine the cause. A biopsy is commonly recommended to rule out precancerous changes, involving the removal of a small tissue sample for laboratory analysis. This quick, straightforward procedure helps identify whether the cells show signs of concern.
Additional diagnostic steps may include:
- Extra testing for hairy leukoplakia, especially if a viral condition is suspected
- Imaging or specialist assessment when needed
- Close monitoring of changes in size, texture, or color
Early diagnosis ensures that any potentially harmful developments are addressed promptly. Routine check-ups with a dental professional or a hygienist in Chichester also support long-term monitoring and early detection of new or evolving patches.
Treatment Options
1. Lifestyle and Habit Changes
The first step in managing leukoplakia often involves removing the source of irritation. This may include:
- Stopping smoking or chewing tobacco
- Reducing alcohol intake
- Improving daily oral hygiene practices
For many people, simply eliminating the irritant leads to noticeable improvement or complete resolution of the patches.
2. Dental and Medical Interventions
If leukoplakia is caused by irritation from a sharp tooth or poorly fitting denture, adjustments or replacements may be needed. Hairy leukoplakia may require medication, especially when linked to viral or immune issues. Sudden discomfort, bleeding, or rapid changes should prompt a visit to an emergency dentist in Chichester.
3. Surgical Treatments
If a biopsy reveals dysplasia or if the patches become particularly large or concerning, removal may be recommended. This can be done through:
- Laser therapy
- Cryotherapy (freezing the tissue)
- Traditional surgical excision
These procedures are typically quick and carried out under local anaesthesia, offering reassurance and protection against further risk.
Can Leukoplakia Turn Into Cancer?
Although most cases of leukoplakia remain harmless, a small number can develop into oral cancer over time. Factors that increase this risk include:
- Red patches mixed with white (erythroplakia)
- Rapid growth of the patch
- Persistent soreness or pain
- A long history of smoking and drinking
This is why regular monitoring is essential. With professional guidance and periodic check-ups, any suspicious changes can be caught early, significantly reducing long-term risk.
Prevention Tips
Good oral health habits are key to lowering your risk of developing leukoplakia. Consider the following preventive strategies:
| Preventive Action | Benefit |
| Quit smoking/tobacco | Reduces irritation and cancer risk |
| Limit alcohol use | Protects oral tissues |
| Address dental issues promptly | Prevents chronic friction |
| Maintain strong oral hygiene | Promotes healthier tissue |
| Attend regular dental check-ups | Ensures early detection |
A balanced diet, hydration and regular cleanings can further help maintain healthy oral tissues and reduce irritation.
When to See a Dental Professional
You should seek professional advice if:
- A white or grey patch lasts longer than two weeks
- There is persistent pain, discomfort or bleeding
- The patch changes shape, size or color
- You are a long-term smoker or drinker and notice new symptoms
Early assessment ensures greater peace of mind and more effective treatment options.
Conclusion
Leukoplakia may be a common condition, but paying attention to changes in your oral health is crucial. While most cases remain harmless, staying aware of symptoms, eliminating risk factors and seeking timely professional advice can significantly reduce complications. With the support of experienced dental professionals and proactive habits, you can maintain long-term oral health and confidence. For reliable care and regular check-ups, you can always count on Chichester to guide you toward better oral health and peace of mind.
Care
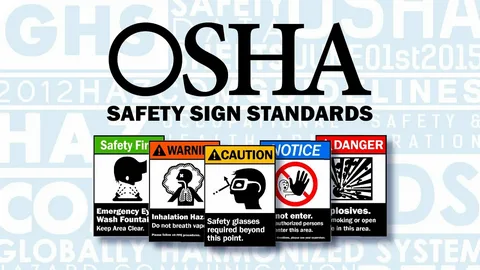
Enhance Your Career with the OSHA Industrial Safety Course
Introduction
Safety at work is a need in the contemporary industrial and construction industries which are experiencing rapid expansion. The manufacturing sectors also require skilled workers who are conversant with the international safety measures as well as preventing accidents before they occur. This is whereby the OSHA Industrial Safety Course in Rawalpindi comes in.
United College of Technology is pleased to provide a single and career oriented OSHA course in Rawalpindi that is intended to incorporate the current industry demand and global safety measures. This course is best suited to students, individuals, and organizations that would wish to enhance workplace safety and compliance.
What Is OSHA and Why Is It Important?
OSHA is an acronym of Occupational Safety and Health Administration, which is an internationally acclaimed author that establishes the safety standards in the places of work. OSHA guidelines have been used to minimize workplace hazards, injuries, and in favor of a robust safety culture in industries like:
- Construction
- Manufacturing
- Oil & Gas
- Engineering
- Power Plants
- Factories and Warehouses
Students can obtain real knowledge about rules of industrial safety which are recognized in the world by attending an OSHA course in Rawalpindi.
OSHA Industrial Safety Course in Rawalpindi – Course Overview.
United College of Technology provides the OSHA Industrial Safety Course in Rawalpindi that concentrates on the practical aspects of safety concerns in an industrial setting. The course involves both theoretical and practical studies to make sure that everything is understood.
Key Learning Areas Include:
- Detection of hazards in industries.
- Risk evaluation and management.
- The prevention of accidents at work.
- Safety signs and symbols
- Personal Protective Equipment (PPE).
- Fire and emergency response.
- Safety of electricity and mechanical.
- Standards of health and environmental safety.
The course is an OSHA in Rawalpindi course which is appropriate to both the novice and the already established professionals in need of certification regarding safety.
Why United College of Technology to take OSHA Course in Rawalpindi?
The selection of the appropriate institute is of important concern to quality education and progress of career. United College of technology is among the most reputable technical colleges that provide professional courses in terms of safety in the city of Rawalpindi.
The advantages of studying at United College of Technology are as follows:
- Well trained, professional teachers.
- Industry-relevant curriculum
- On-the-job training model.
- Affordable course fees
- Recognized OSHA certification.
- Career guidance and support
We would like to have qualified safety professionals who are capable of fulfilling both local and international industry requirements.
Career Scope Following OSHA Industrial Safety Course.
On finishing the OSHA Industrial Safety Course in Rawalpindi, students have an opportunity to take different jobs in the sphere of safety in Pakistan and other countries.
Career Opportunities It includes:
- Safety Officer
- Supervisor of industrial safety.
- HSE Officer
- Site Safety Inspector
- Safety Coordinator
- Health and Safety Manager (experienced).
The OSHA-certified professionals are in high demand particularly in the construction work, factories, and multinational enterprises.
Who Can enroll in OSHA Course in Rawalpindi?
The course is an OSHA program in Rawalpindi that is accessible to a large group of learners, and they include:
- Fresh students
- Diploma holders
- Engineers
- Site supervisors
- Technicians
- Factory workers
- Safety professionals
There is no higher education level needed and this is why it is easy to use and accessible to any person interested in workplace safety.
Experiential Training and Industry-Based Learning.
We are of the opinion that theory is not as valuable as practice is at United College of Technology. The OSHA Industrial Safety Course of Rawalpindi has real life case studies, safety drills and analysis of hazards to equip the students with the real work conditions.
Such practical method enables students to be able to use safety regulations with a lot of confidence in their job sites and industrial workplaces.
The importance of OSHA Certification in Pakistan and Europe.
The employers nowadays are attracted to the candidates who have professional safety certification. An OSHA course in Rawalpindi is not only one that is going to enhance your knowledge of safety but also improve your CV and employment opportunities.
The certification of OSHA demonstrates that you:
- Know the international standards of safety.
- Can reduce workplace risks
- Trained to deal with emergencies.
- Appreciate health and safety compliance.
- That would make you a valuable investment in any company.
Conclusion
The industrial Safety Course provided by the OSHA in Rawalpindi by United College of Technology is a good chance to have a good career in industrial and workplace safety. As more industry expands, the need to have professional safety workers is more than ever.
Studying this OSHA course in Rawalpindi you obtain internationally accepted knowledge, practical skills and get better employment opportunities not only in Pakistan but also in the abroad. United College of Technology is the place to begin in case you are serious about safety, professionalism and career development.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom































