Uncategorized
Reviewing Your Options in Light of Recent Cancer Treatment Advances
A cancer diagnosis can be distressing, but there is reason for hope thanks to advances in science and medicine. Numerous cancer survivors’ stories highlight the value of a well-thought-out treatment program. As novel cancer treatments are being developed at a rapid rate, patients today have more choices than ever before. Immunotherapy and other targeted pharmaceutical medications may be part of these treatments, which could result in remission or perhaps a cure. Here, we’ll examine the current landscape of cancer treatment options and have an open conversation about how they could be used to help people cope with and ultimately overcome this awful disease.
Surgery
It’s important to remember that there are many different surgical options for treating cancer. The optimal surgical strategy for each given patient depends on a number of criteria, including the type and stage of the cancer, the patient’s overall condition, and the surgeon’s level of experience.
The following are some of the more common surgical procedures performed for cancer patients.
A lumpectomy is surgery to remove a breast tumor. This method is also known as a “partial mastectomy.” Lumpectomy is a common surgical treatment for treating breast cancer in its early stages.
A mastectomy is the surgical removal of both of a woman’s breasts. A mastectomy is an option for women with advanced breast cancer.
Surgery to remove the prostate gland is called a prostatectomy. A prostatectomy is commonly prescribed for men who have been diagnosed with prostate cancer at an early stage.
Radiation therapy uses X-rays and other high-energy radiation sources to eradicate cancer cells. Both external radiation therapy devices and radioactive materials implanted at or near the tumor are viable options for delivering radiation therapy.
Chemotherapy
Chemotherapy refers to the use of drugs in the treatment of cancer. Chemotherapy is not limited to intravenous (IV) use; it can either be ingested or applied topically (as a cream or ointment). It is often delivered in cycles, with each cycle including both a treatment period and a recovery phase. It is usual practice to combine chemotherapy with other treatments.
Weakness, nausea, vomiting, hair loss, mouth sores, and a heightened susceptibility to infection are just some of the unpleasant side effects of chemotherapy. Some people may develop extremely serious adverse effects, such as organ failure or an allergic reaction.
Chemotherapy is not appropriate for all patients with cancer. Your doctor will think carefully about your overall health, the specifics of your disease, and the results you want to achieve before recommending chemotherapy as a treatment.
Radiosurgery
In order to eradicate malignant tissue, radiosurgery is used as a treatment option. The radiation therapy only affects the tumor, sparing the surrounding healthy tissue. Therefore, radiosurgery is highly effective for patients with low-grade, locally-confined cancers.
Radiosurgical patients can often return home the same day they were treated. A typical day can be resumed after less than an hour of downtime is required. The time needed to recuperate could range from a few days to a few weeks, depending on the size and location of the tumor.
Dr. Gil Lederman heads up a top-notch New York cancer radiosurgery center.
Immunotherapy
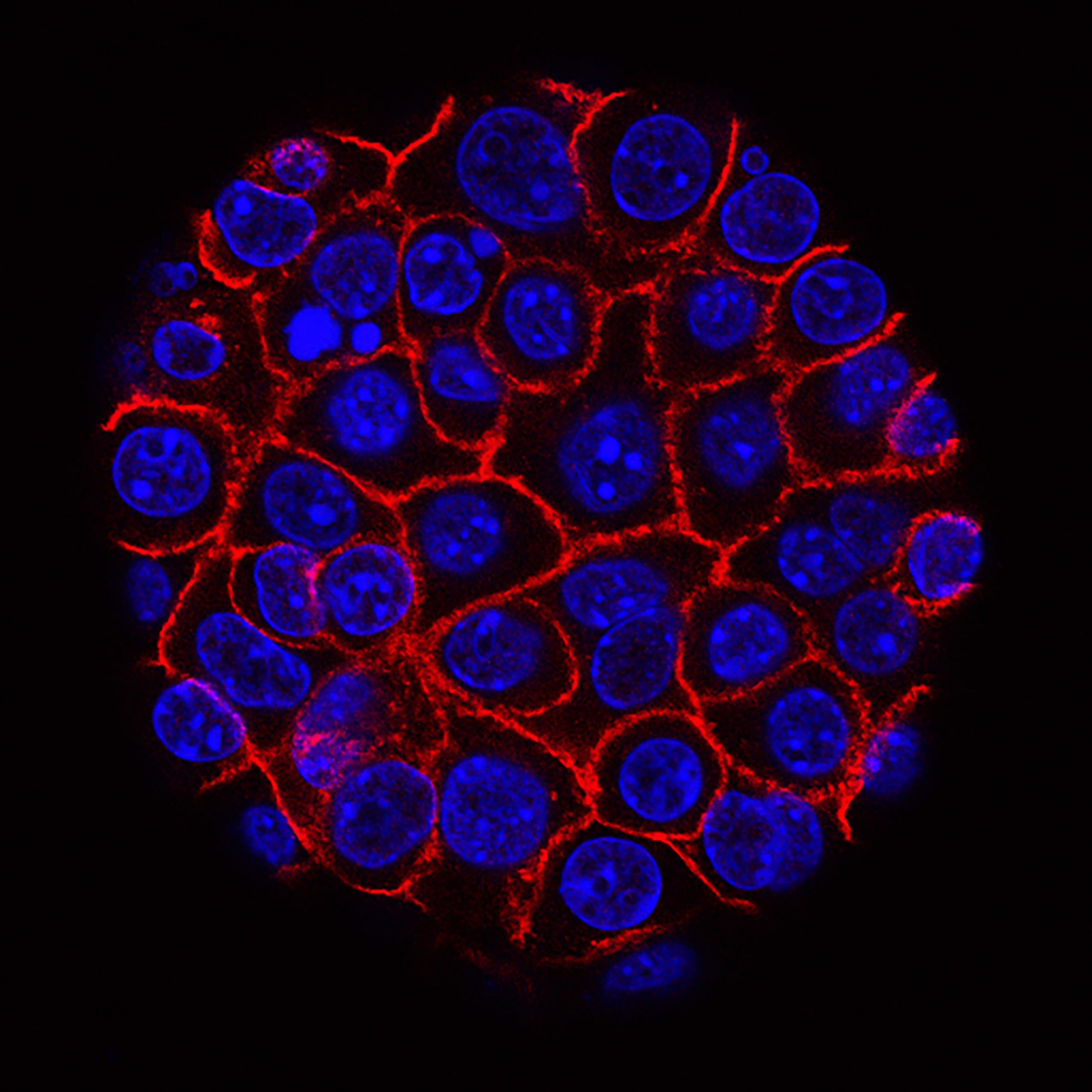
Immunotherapy’s success in human studies as a fresh approach to cancer treatment is exciting. With immunotherapy, a patient’s immune system is boosted in an effort to speed up the natural death rate of cancer cells. There are a number of immunotherapies available, and they each have their own unique mechanism of action.
Using checkpoint inhibitors, immunotherapists disable proteins that act as immune system brakes. The immune system’s capacity to recognize cancer cells and destroy them is thereby enhanced. Checkpoint inhibitors have shown promise in the treatment of melanoma and lung cancer, and their utility in combating other cancers is also being investigated.
In adoptive cell therapy, the patient’s own immune cells are employed after being separated and modified in the lab to be more effective against cancer cells. The modified cells are reintroduced to the patient so that their immune system can better combat cancer. The effectiveness of adoptive cell therapy in the treatment of various cancers is now being investigated in clinical trials.
Immunotherapy is a relatively new area of cancer study with enormous potential to improve patients’ outcomes.
Care That Is Specifically Intended
The purpose of targeted therapy in the treatment of cancer is to block the activity of one or more individual chemicals or genes that promote tumor growth and spread. It is usual practice to combine this therapy with other cancer treatments. Targeted therapy has the potential to kill cancer cells more effectively while minimizing damage to healthy tissue.
Human Subjects Experimentation in the Health Sciences
Patients with cancer now have many therapeutic options thanks to clinical trials. The general public needs to be aware that novel cancer treatments are being tried in clinical trials.
Clinical trials, like any other scientific endeavor, can have a wide range of aims, time frames, and organizational structures. While other clinical trials investigate novel treatments that have not yet been made available to the public, others examine tried-and-true methods for the first time in regard to a specific cancer or group of cancers. Clinical trials are a useful tool for evaluating new approaches to cancer prevention, screening, and diagnosis.
Clinical trials are conducted by researchers in a wide variety of settings, from academic medical centers and government research institutes to private practices and community health clinics. It may take quite some time after a medicine has undergone extensive testing in the lab before it is ready to be tested on human volunteers in a clinical study.
If you’re a cancer patient contemplating about taking part in a trial, you and your doctor should talk about the pros and cons. Clinical trials aren’t always the most effective path of treatment because each patient’s disease is unique. Nonetheless, clinical trials are some patients’ greatest bet for receiving a successful medicine.
Assistance Provided
Cancer patients have access to a wide variety of treatment options, and determining which one would be most successful for them requires consideration of their individual needs. But supportive care, which attempts to reduce symptoms associated with cancer and its treatment, is beneficial for everyone who has the condition.
As part of a bigger network of care, services like pain management, nutritional advice, and emotional support can be offered. In order to get the best possible supportive care, cancer patients should work with a healthcare team that is experienced with their illness.
Those dealing with cancer often experience depression and anxiety. They can receive supportive care to help them cope with these challenges and improve their quality of life overall.
Identifying Your Specific Treatment and Intervention Needs and Learning to Implement Them
Cancer treatment options have improved greatly in recent years. It may be difficult to determine the best course of action to take in your situation. As you weigh your treatment options, keep in mind the following:
In any case, why are we making an attempt to treat it?
Patients with cancer may eventually have to accept illness management as an acceptable alternative to a cure. To what extent you answer this question honestly will help establish the best therapeutic approach to take with you.
Please tell me how dangerous this treatment is.
There may be some unwanted side effects with every treatment you choose. Symptoms might range from annoying to life-threatening. Think about the potential adverse reactions the treatment could cause.
The most pressing question is how long will I have to go through this therapy.
Treatments can be utilized in either a short-term or long-term capacity. Consider how much time you can realistically dedicate to treatment before beginning.
Do you have any idea how much money would be needed for something like this to be done in a hospital?
The cost of cancer treatment can quickly add up. Before deciding to pursue therapy, one should assess their financial circumstances.
Conclusion
As a result, there are now many more cancer treatments available to people today. Developing a treatment plan for a patient requires consideration of their unique requirements (which may include anything from surgery and chemotherapy to radiation and immunotherapy to targeted drugs). You should know what kinds of treatments are out there so you can pick the one that’s ideal for you. If you feel you need help, it’s important to talk to your doctor or health care team, who may provide personalized recommendations for you depending on your condition and other considerations.
Uncategorized
Global Flow Meters Market Analysis: Trends and Projections

The global flow meters market is experiencing notable growth, with a valuation estimated at USD 8.29 billion in 2024. Projections indicate this figure will rise steadily, reaching approximately USD 13.77 billion by 2033, exhibiting a compound annual growth rate (CAGR) of 5.80% from 2025 to 2033. This growth trajectory underlines the increasing importance of flow measurement technologies across various industries.
Understanding the Flow Meters Market
According to a report by Straits Research, a thorough analysis of the flow meters market provides valuable insights into its overall structure, essential dynamics, and future potential. The report meticulously evaluates different market segments, offering reliable forecasts to aid strategic decision-making.
To ensure the depth and accuracy of the analysis, the study employs a balanced approach, combining both primary and secondary research methodologies.
Research Methodology
Primary research components include expert interviews, surveys, and direct interactions within the industry, while secondary research draws on reputable sources such as industry reports, company publications, and governmental databases.
This rigorous methodology helps to capture a holistic view of the market, offering stakeholders a dynamic perspective of current and prospective trends.
What is the Market’s Scope?
The report delves into the various applications of flow meters, spotlighting key market players including established industry leaders, emerging companies, and new entrants. It employs analytical frameworks like PORTER’s Five Forces and PESTEL analysis to evaluate both micro- and macroeconomic factors influencing the market.
Advanced statistical tools are utilized to identify trends and growth estimations, thereby informing competitive positioning for existing and prospective players.
Regional Analysis of the Flow Meters Market
The regional breakdown of the flow meters market is critical for understanding its dynamics across various geographic areas, including North America, Europe, Asia Pacific, Latin America, and the Middle East and Africa. Each region’s performance is evaluated based on key indicators such as market size, growth rates, consumption patterns, and trade activities.
By dissecting regional variations, the report highlights distinct drivers, challenges, and spatial growth prospects influencing the overall landscape of the flow meters market.
Market Segmentation
By Technology
The market can be categorized based on various technologies employed in flow measurement, including:
- Coriolis
- Electromagnetic
- Differential Pressure
- Ultrasonic
- Positive Displacement
- Turbine
- Magnetic (In-Line, Insertion, Low Flow)
- Vortex
- Others
By End-User
Different industries utilize flow meters for various applications, such as:
- Water & Wastewater
- Refining & Petrochemical
- Oil & Gas
- Chemical
- Power Generation
- Pulp & Paper
- Food & Beverage
- Pharmaceuticals
- Metals & Mining
- Others
By Application
Flow meters find applications across diverse sectors, including:
- Water & Wastewater
- Oil & Gas
- Chemicals
- Power Generation
- Pulp & Paper
- Food & Beverage
- Others
By Type
In terms of functionality, flow meters may be classified as:
- Electric
- Solar
- Battery Powered
By Size
The size of flow meters also differentiates them within the market, with categories including:
- 2 inches
- 4 inches
- 6 inches
- More than 6 inches
Key Players in the Flow Meters Market
Numerous companies are key contributors to the dynamics of the flow meters market, including:
- Yokogawa Electric Corporation
- ABB Ltd.
- Siemens AG
- Bronkhorst High-Tech BV
- Honeywell International Inc.
- SICK AG
- Omega Engineering Inc. (Spectris PLC)
- Christian Bürkert GmbH & Co. KG
- TSI Incorporated
- Keyence Corporation
- Emerson Electric Co.
- Sensirion AG
- Azbil Corporation
- Endress+Hauser AG
- KROHNE Messtechnik GmbH
Key Questions Addressed in the Flow Meters Market Report
The report answers critical questions relevant to stakeholders looking to navigate this vibrant market landscape:
- What does the flow meters market represent, and how is it utilized across different industries?
- What was the flow meters market size in 2025?
- What CAGR is anticipated for the flow meters market during the projection period?
- What are the pivotal factors driving growth in the flow meters market?
- How is the flow meters market segmented, and what notable sub-segments exist?
- What strategies are market players implementing for expansion and growth?
- What new applications and trends are emerging within the flow meters market?
- Which market segments are expected to witness the highest rates of growth?
- Who are the leading companies in the flow meters market, and what solutions do they offer?
- What factors are shaping competition in the flow meters market?
What the Flow Meters Market Report Provides
The report offers a thorough analysis covering:
- Historical market sizes and competitive landscapes
- Trends in pricing and regional price curves
- Market size, shares, and forecasts segmented by type and region
- Dynamics such as drivers, restraints, opportunities, and key trends across regions
- Detailed market segmentation, including sub-segments and geographical insights
- Competitive analysis highlighting leaders, followers, and regional contenders
- Strategic company profiles alongside competitive benchmarking
- PESTLE and PORTER’s Five Forces analyses
- Assessments of the value chain and supply chain
- Legal and regulatory analyses pertinent to different regions
- SWOT analysis highlighting lucrative business opportunities
- Strategic recommendations tailored for market participants
About Straits Research
For over a decade, Straits Research has collaborated with more than 2,000 organizations worldwide, providing data-driven insights that empower both SMEs and large enterprises to traverse intricate and evolving markets confidently. The firm publishes comprehensive market reports across various high-impact industries, enabling businesses to identify growth opportunities, mitigate risks, and make well-informed strategic decisions.
By offering actionable insights, Straits Research supports decision-makers in the flow meters market and beyond, making it a trusted source for market intelligence.
Uncategorized
Tesla Rental Dubai Airport: Elevate Your Travel Experience in Style

Dubai is a city known for innovation, luxury, and unforgettable travel experiences. Whether you’re visiting for business, leisure, or a stopover, one of the best ways to elevate your journey is by choosing a Tesla rental Dubai airport service.
Sleek, powerful, and fully electric, Teslas are redefining how travelers explore the UAE. From zero-emission driving to advanced autopilot features, Tesla delivers an unmatched travel experience the moment you land at Dubai International Airport (DXB).
In this guide, you’ll discover everything you need to know before booking a Tesla—from available models and rental requirements to pricing, benefits, and why renting at Dubai Airport is the smartest choice.
Why Choose Tesla Rental Dubai Airport?
Renting a Tesla directly from Dubai Airport provides convenience, comfort, and style—all in one package. Instead of waiting for taxis or relying on public transport, you get a premium electric vehicle ready as soon as you step outside the arrival terminal.
Here’s why travelers prefer a Tesla rental Dubai airport service:
1. Immediate Pickup & Easy Process
No hassle, no long queues. Your Tesla will be waiting at the airport, cleaned, charged, and ready to drive. This saves time and offers a smooth travel start.
2. Futuristic Driving Experience
Dubai is the perfect city for modern travel. Tesla’s autopilot mode, long-range battery, and high-tech features fit Dubai’s advanced road infrastructure.
3. Environment-Friendly Travel
Dubai encourages sustainable transportation. Using a Tesla means zero carbon emissions and a clean driving experience without compromising on power.
4. Affordable Luxury
Compared to other luxury car brands, Tesla offers premium performance at surprisingly competitive rental prices.
Top Tesla Models You Can Rent at Dubai Airport
A Tesla rental Dubai airport service usually includes multiple models, so you can choose the one that fits your needs:
Tesla Model 3
- Perfect for premium yet budget-friendly travel
- Fast acceleration and long-range battery
- Great for couples or solo business travelers
Model Y
- Spacious interior
- Ideal for small families or long drives across Dubai
Tesla Model S
- High performance
- Luxurious interior
- A favorite among business executives
Model X
- Falcon-wing rear doors
- Exceptional comfort
- Best for families and group travelers
Whether you’re heading to Downtown Dubai, Marina, or Palm Jumeirah, Tesla ensures you reach your destination quickly, quietly, and safely.
Benefits of Choosing Tesla Over Traditional Cars
Why is Tesla rental Dubai airport becoming the top choice among tourists and locals?
Here’s what makes Tesla stand out:
1. Advanced Autopilot
Enjoy stress-free driving with lane-keeping, smart cruise control, and automatic braking.
2. Instant Power
Tesla’s electric motors offer instant torque, giving a smooth and powerful acceleration.
3. Charging Convenience
Dubai has hundreds of EV charging stations, especially near malls, hotels, and major attractions.
4. Safety First
Tesla vehicles consistently rank among the safest cars in the world, thanks to advanced sensors and AI-powered features.
5. Silent & Smooth Ride
Unlike petrol cars, Teslas offer a quiet cabin and a calm driving experience.
How Much Does a Tesla Rental Dubai Airport Cost?
The price depends on the model, duration, and rental company. Here’s a general breakdown:
| Tesla Model | Daily Price (Approx.) |
|---|---|
| Tesla Model 3 | AED 350 – AED 550 |
| Tesla Model Y | AED 450 – AED 700 |
| Tesla Model S | AED 700 – AED 1,200 |
| Tesla Model X | AED 900 – AED 1,500 |
Long-term rentals usually come with discounted rates.
Requirements for Tesla Rental at Dubai Airport
To book a Tesla rental Dubai airport, you will need:
For Tourists
- Passport copy
- International Driving Permit (IDP)
- Valid home country license
- Visa copy
- Security deposit
For UAE Residents
- Emirates ID
- UAE driving license
- Security deposit
Most rental companies accept credit cards, debit cards, and even cash deposits.
Where Can You Drive Your Tesla in Dubai?
Dubai is full of iconic places that look even better when you’re driving a Tesla. Some must-visit spots include:
- Burj Khalifa & Downtown Dubai
- Dubai Marina & JBR
- Palm Jumeirah
- Dubai Mall
- The Museum of the Future
- Desert roads heading toward Abu Dhabi
Tesla’s excellent navigation system makes exploring the city extremely easy.
Charging Your Tesla in Dubai
With a Tesla rental Dubai airport, charging is hassle-free. Dubai offers:
Tesla Superchargers
Fast charging—80% in around 30 minutes.
DEWA EV Green Chargers
Located widely across the city.
Mall & Hotel Chargers
Common in luxury hotels and shopping malls.
Most rental companies provide you with charging maps and instructions.
Why Rent Tesla at Dubai Airport Instead of City Branches?
Here are the benefits of choosing airport pickup:
- No waiting time
- Immediate access upon landing
- No need for taxis or public transport
- Saves money on additional pickup fees
- Best availability of Tesla models
Airport rentals are perfect for quick business trips, short holidays, or long stays.
Tips for Getting the Best Tesla Rental Deals
To get the best price on a Tesla rental Dubai airport, follow these tips:
- Book at least 1–2 weeks in advance
- Compare prices across rental companies
- Look for discounts on long-term rentals
- Avoid last-minute bookings during peak season
- Check mileage limits before confirming
Final Thoughts
Dubai sets the standard for innovation and luxury—and Tesla fits perfectly into this modern lifestyle. Choosing a Tesla rental Dubai airport service gives you instant comfort, premium performance, and eco-friendly travel from the moment you land.
With smooth acceleration, advanced technology, and unmatched convenience, Tesla is more than a car—it’s an experience.
Whether you’re here for business or exploring the city’s wonders, renting a Tesla ensures you enjoy a futuristic, stylish, and hassle-free ride throughout your stay.
Uncategorized
How to Maintain a 4R70W Transmission for Longevity

Introduction
The 4R70W transmission is a popular automatic transmission used in many Ford vehicles. Known for its durability and performance, it can last for hundreds of thousands of miles if properly maintained. However, neglecting maintenance can lead to slipping gears, overheating, or complete transmission failure. Maintaining a 4R70W transmission requires regular fluid checks, proper servicing, and understanding common issues. This guide will help you learn practical steps to keep your 4R70W transmission running smoothly for years, saving money and avoiding costly repairs.
Understanding the 4R70W Transmission
The 4R70W is a four-speed automatic transmission with electronic controls. It is used in various Ford models, including the Mustang, Explorer, and F-Series trucks. The “W” in the name stands for “wide ratio,” which provides better acceleration and fuel efficiency.
Key features include:
- Electronically controlled shifting for smoother gear changes
- Wide gear ratios for balanced performance and fuel economy
- Durable internal components designed for longevity when properly maintained
Despite its reliability, the 4R70W transmission can face issues if fluid levels are low, filters are clogged, or electronic controls malfunction. Understanding how it works helps in maintaining it effectively.
Importance of Regular Transmission Maintenance
Regular maintenance is crucial for the longevity of the 4R70W transmission. Poor maintenance can result in:
- Overheating, which damages internal components
- Gear slippage, causing performance issues
- Contaminated transmission fluid, leading to wear and tear
- Complete transmission failure, which is expensive to repair
Routine maintenance ensures smooth operation, reduces repair costs, and extends the life of the transmission.
Key Steps to Maintain a 4R70W Transmission
1. Check Transmission Fluid Regularly
- Transmission fluid lubricates the gears, controls temperature, and keeps the system clean. Checking fluid levels monthly is essential. Low or dirty fluid can cause overheating and slipping.
- Locate the transmission dipstick while the vehicle is warm and idling.
- Check the fluid level and color. Healthy fluid is usually red or pink.
- If the fluid is dark brown or smells burnt, it needs to be replaced immediately.
2. Change Transmission Fluid and Filter
- Replacing the fluid and filter ensures the transmission stays clean and performs efficiently. Ford recommends changing the fluid every 30,000 to 60,000 miles, depending on driving conditions.
Steps include:
- Draining old fluid
- Replacing the transmission filter
- Refilling with the correct type of automatic transmission fluid (ATF)
3. Inspect and Replace Seals
- Seals prevent leaks and maintain proper fluid levels. Inspect transmission pan and output shaft seals regularly for signs of leakage. Replace worn or damaged seals promptly to avoid low fluid levels.
4. Monitor Transmission Temperature
- Overheating is one of the main causes of transmission failure. Keep an eye on the transmission temperature, especially during towing or heavy-duty use. Installing an auxiliary transmission cooler can help prevent overheating.
5. Avoid Aggressive Driving
- Rapid acceleration, hard braking, and sudden gear changes put extra stress on the transmission. Smooth driving habits reduce wear and tear on internal components.
6. Use the Correct Transmission Fluid
- Using the wrong type of ATF can damage the transmission. Always refer to the owner’s manual or manufacturer’s recommendation to ensure the correct fluid type and specifications.
7. Check Transmission Mounts
- Transmission mounts hold the transmission in place. Worn or broken mounts can cause vibration, misalignment, and stress on the transmission. Inspect mounts regularly and replace if needed.
8. Keep the Cooling System in Check
- The transmission relies on the vehicle’s cooling system to maintain proper operating temperatures. Ensure the radiator and coolant levels are sufficient. A well-maintained cooling system prevents overheating and prolongs transmission life.
9. Software Updates and Electronic Checks
- Modern 4R70W transmissions use electronic controls. Occasionally, Ford releases software updates to improve shifting performance or fix minor issues. Consult your dealer for updates and diagnostic checks.
10. Listen for Warning Signs
- Pay attention to unusual noises, slipping gears, or delayed shifting. Early detection of problems allows for timely repairs and prevents major failures.
Common Issues with 4R70W Transmission
Even with proper maintenance, some common issues can arise:
- Shift Flare: The transmission may briefly increase engine RPM before downshifting. Often caused by worn clutches or low fluid.
- Hard Shifting: Stiff or delayed gear changes can indicate a problem with solenoids or fluid levels.
- Torque Converter Problems: Can cause shuddering or slipping, requiring inspection and possibly replacement.
- Overheating: Common when towing or driving in hot conditions. Proper fluid and cooling maintenance prevent this.
Addressing these issues early through routine maintenance can extend the transmission’s life and reduce repair costs.
Tips for Long-Term Transmission Care
- Regular Inspections: Have a certified mechanic inspect the transmission periodically to detect early signs of wear or leaks.
- Follow Manufacturer Service Schedule: Stick to Ford’s recommended maintenance schedule for fluid changes, filter replacements, and inspections.
- Avoid Overloading the Vehicle: Excess weight strains the transmission. Avoid exceeding the vehicle’s towing and payload limits.
- Drive Smoothly: Gentle acceleration, braking, and gear changes reduce stress on the transmission and extend its lifespan.
- Store Properly During Long Periods of Inactivity: If the vehicle will be idle for an extended period, ensure the transmission fluid is topped up and consider using a transmission stabilizer to prevent corrosion and seal drying.
Benefits of Maintaining a 4R70W Transmission
- Extended Lifespan: Proper maintenance ensures the transmission lasts longer.
- Reduced Repair Costs: Preventative care avoids expensive major repairs.
- Improved Performance: Smooth shifting and consistent operation enhance driving experience.
- Better Fuel Efficiency: A well-maintained transmission reduces energy loss and improves mileage.
- Peace of Mind: Knowing your transmission is in good condition prevents unexpected breakdowns.
Conclusion
Maintaining a 4R70W transmission is essential for ensuring reliability, performance, and longevity. Regular fluid checks, timely filter replacements, seal inspections, and careful driving habits all contribute to a healthy transmission. Monitoring temperature, using the correct fluid, and keeping the cooling system in check prevent overheating and damage. By following these steps and addressing issues promptly, drivers can enjoy smooth gear shifts, reduced repair costs, and extended transmission life. Proper maintenance is the key to maximizing the investment in your vehicle’s 4R70W transmission and avoiding costly problems in the future.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom































