health
Importance of Exercise: Unveiling Its Benefits and Best Practices

Introduction
Exercise is a fundamental aspect of maintaining and improving overall health. In today’s fast-paced world, it is more crucial than ever to understand the significance of regular physical activity. Engaging in exercise provides numerous benefits, including physical fitness, mental well-being, and enhanced quality of life. This article delves into the multifaceted benefits of exercise, exploring the recommended types and providing a comprehensive guide to incorporating physical activity into daily routines.
Types and Categories of Exercise

Image by: Yandex.com
1. Cardiovascular Exercise
Cardiovascular or aerobic exercise involves activities that increase the heart rate and promote cardiovascular endurance. Examples include running, cycling, swimming, and brisk walking.
2. Strength Training
Strength training focuses on building muscle mass and strength. It includes exercises like weightlifting, resistance band exercises, and bodyweight workouts such as push-ups and squats.
3. Flexibility Exercises
Flexibility exercises enhance the range of motion of muscles and joints. Common flexibility activities include stretching routines, yoga, and Pilates.
4. Balance Exercises
Balance exercises improve stability and prevent falls, especially important for older adults. Activities such as tai chi and specific balance drills are beneficial.
5. High-Intensity Interval Training (HIIT)
HIIT involves short bursts of intense activity followed by rest or low-intensity exercises. It is highly effective for burning calories and improving cardiovascular health.
6. Low-Impact Exercises
Low-impact exercises are gentle on the joints and suitable for individuals with injuries or chronic conditions. Examples include swimming, cycling, and elliptical training.
Symptoms and Signs of a Sedentary Lifestyle
1. Weight Gain
A sedentary lifestyle often leads to weight gain due to reduced calorie expenditure.
2. Decreased Muscle Mass
Lack of physical activity results in muscle atrophy and decreased strength.
3. Increased Fatigue
Sedentary individuals frequently experience higher levels of fatigue and reduced energy.
4. Poor Cardiovascular Health
Lack of exercise contributes to poor cardiovascular health, increasing the risk of heart disease.
5. Mental Health Issues
Physical inactivity is linked to higher rates of depression, anxiety, and other mental health conditions.
Causes and Risk Factors of Inactivity
1. Technological Advances
The rise of technology has led to more sedentary jobs and leisure activities.
2. Urbanization
Urban environments often lack accessible spaces for physical activity.
3. Lifestyle Choices
Busy schedules and a preference for passive entertainment contribute to inactivity.
4. Health Conditions
Chronic illnesses and disabilities can limit the ability to engage in physical activity.
5. Lack of Education
A lack of knowledge about the benefits of exercise and how to incorporate it into daily life is a significant barrier.
Diagnosis and Tests for Physical Fitness
1. Body Mass Index (BMI)
BMI is a common measure to assess if an individual’s weight is appropriate for their height.
2. Cardiovascular Fitness Tests
Tests such as the treadmill stress test evaluate cardiovascular health and endurance.
3. Strength and Flexibility Assessments
Strength and flexibility are assessed through various physical tests like grip strength and sit-and-reach tests.
4. Comprehensive Physical Exam
A full physical exam by a healthcare provider can identify underlying conditions affecting fitness levels.
Treatment Options: Incorporating Exercise into Daily Life
1. Developing a Routine
Establishing a regular exercise schedule is crucial for consistency.
2. Setting Realistic Goals
Goals should be specific, measurable, achievable, relevant, and time-bound (SMART).
3. Seeking Professional Guidance
Personal trainers and physical therapists can provide tailored exercise programs.
4. Utilizing Technology
Fitness apps and wearable devices can track progress and provide motivation.
5. Community Support
Joining exercise groups or classes can provide social support and accountability.
Preventive Measures: Staying Active

Image by: Yandex.com
1. Daily Activity Goals
Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week.
2. Incorporating Movement into Daily Tasks
Use stairs instead of elevators, walk or bike for short trips, and take breaks to stand or walk during sedentary activities.
3. Promoting Physical Education
Schools and workplaces should encourage physical activity through programs and facilities.
4. Public Health Campaigns
Government and organizations should promote awareness of the benefits of exercise.
5. Creating Active Environments
Design urban spaces to encourage walking, cycling, and outdoor activities.
Personal Stories or Case Studies
1. Success Stories
Real-life examples of individuals who transformed their health through exercise.
2. Overcoming Obstacles
Stories of people who overcame challenges such as chronic illness or busy schedules to stay active.
3. Inspiring Testimonials
Testimonials from individuals who found joy and fulfillment in regular physical activity.
Expert Insights
1. Medical Professionals
Quotes and advice from doctors and physical therapists on the importance of exercise.
2. Fitness Experts
Insights from personal trainers and fitness coaches on effective exercise routines.
3. Nutritionists
Advice on how diet and exercise work together to enhance health.
4. Mental Health Professionals
Perspectives on how exercise positively impacts mental health.
Conclusion
Regular exercise is vital for maintaining physical and mental health. It reduces the risk of chronic diseases, enhances mental well-being, and improves overall quality of life. By understanding the various types of exercise and incorporating them into daily routines, individuals can achieve significant health benefits. It is essential to overcome barriers to physical activity and make exercise an integral part of daily life.
FAQs
What are the main benefits of regular exercise?
Regular exercise improves cardiovascular health, builds and maintains muscle mass, enhances flexibility, and promotes mental well-being.
How often should I exercise?
Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week, combined with muscle-strengthening activities on two or more days a week.
Can exercise help with weight loss?
Yes, exercise helps burn calories and build muscle, which can lead to weight loss when combined with a healthy diet.
What type of exercise is best for beginners?
Beginners should start with low-impact exercises like walking, swimming, or cycling, and gradually incorporate strength training and flexibility exercises.
How can I stay motivated to exercise regularly?
Setting realistic goals, tracking progress, finding a workout buddy, and varying your exercise routine can help maintain motivation.
Is it safe to exercise if I have a chronic condition?
Consult with your healthcare provider before starting any new exercise program, especially if you have a chronic condition. They can help create a safe and effective exercise plan.
Care
Preventive Health in a Fast World: Comprehensive Approach

Understanding Health in a Fast-Paced World
In our increasingly busy lives, prioritizing health can sometimes feel like a challenge. Between work, family, and social obligations, many people struggle to maintain a balanced lifestyle. However, staying informed and proactive about well-being is crucial for long-term vitality. With the abundance of health information available online, it can be difficult to discern what is reliable and actionable. Trusted sources that provide clear, evidence-based guidance help readers navigate the complexities of nutrition, fitness, mental wellness, and preventive care.
A Reliable Source for Comprehensive Guidance
One platform that has earned recognition for its accessible and well-researched health content is 247healthmag. By offering practical advice, expert insights, and timely updates, it empowers individuals to take charge of their wellness journey.
The platform covers a broad spectrum of topics, including dietary guidance, exercise routines, mental health strategies, and preventive care tips. Its approach ensures that even complex medical and wellness concepts are presented in a way that is understandable and actionable for readers of all backgrounds.

The Importance of Preventive Care
Preventive care is a cornerstone of maintaining long-term wellness. Routine check-ups, screenings, and vaccinations, combined with healthy lifestyle choices, can significantly reduce the risk of chronic illnesses and enhance overall quality of life. Educating oneself about preventive measures allows individuals to address potential health concerns before they escalate.
Reliable health resources emphasize proactive care, highlighting both the physical and mental benefits of early intervention. By adopting a preventive mindset, readers can protect their health while also fostering peace of mind.
Nutrition: The Foundation of Wellness
A well-balanced diet is critical for sustaining energy, supporting immune function, and promoting overall health. Yet, with so many dietary trends and conflicting advice circulating online, it is easy to feel overwhelmed. Trusted platforms break down nutritional science into practical tips that make healthy eating accessible.
From understanding macronutrients and portion control to incorporating nutrient-rich foods into everyday meals, clear guidance empowers individuals to make informed dietary choices. Proper nutrition not only fuels the body but also contributes to improved mood, mental clarity, and long-term vitality.
Mental Health and Emotional Balance for Preventive Care
Physical wellness is only one piece of the puzzle; mental and emotional health are equally important. Stress, anxiety, and burnout are common in today’s fast-paced society, making mental well-being a priority. Expert-driven resources provide strategies for managing stress, practicing mindfulness, and fostering emotional resilience.
They highlight the interconnectedness of mental and physical health, encouraging a holistic approach to overall well-being. By implementing practical mental health practices, readers can improve focus, emotional stability, and quality of life.
The Role of Physical Activity
Regular exercise is essential for maintaining strength, cardiovascular health, and overall fitness. Beyond physical benefits, staying active can enhance mood, reduce stress, and improve sleep quality. Many individuals struggle with knowing where to start or how to sustain an exercise routine.
Credible health platforms offer structured guidance, including beginner-friendly workouts, home exercise options, and tips for staying motivated. By making fitness accessible and enjoyable, these resources help readers integrate physical activity seamlessly into their daily lives.
Building Healthy Habits for Long-Term Wellness
Sustainable health is built on consistent habits. Small, deliberate changes—like drinking more water, prioritizing sleep, or incorporating daily movement—can have a significant impact over time. Trusted platforms provide actionable strategies for cultivating these habits, emphasizing consistency over perfection. By focusing on manageable lifestyle adjustments, individuals are more likely to achieve lasting improvements in both physical and mental well-being.
Staying Informed and Empowered
The digital age offers unparalleled access to health information, but it also comes with the risk of misinformation. Engaging with reliable, expert-reviewed resources ensures that readers receive accurate and timely advice. Staying informed allows individuals to make proactive decisions, adopt preventive care practices, and navigate health challenges with confidence. Knowledge is a powerful tool, and having a dependable source of guidance can be transformative for anyone committed to their wellness journey.
A Holistic Approach to Wellness
True well-being encompasses more than just diet and exercise; it involves nurturing the body, mind, and spirit. High-quality health resources emphasize the integration of sleep, stress management, social connections, and emotional health alongside physical fitness and nutrition. By adopting a holistic perspective, readers can create balance in all aspects of their lives, leading to improved energy, mood, and resilience. Comprehensive guidance encourages thoughtful lifestyle choices that enhance overall quality of life.
Conclusion: Empowering Your Health Journey
In a world overflowing with information, making informed decisions about health is more important than ever. Platforms like 247healthmag provide reliable, evidence-based guidance, empowering readers to take control of their wellness. By combining preventive care, proper nutrition, physical activity, and mental health strategies, individuals can cultivate a balanced and sustainable lifestyle. Access to trustworthy health insights enables readers to confidently navigate their wellness journey, embrace proactive care, and foster long-term vitality. In essence, prioritizing health is not just a choice—it’s an investment in a better, more fulfilling life.
Care
General Physician in Delhi: Dr. Sanchayan Roy for Family Care

Every family has that one member who instinctively knows when something feels “off.” However, just noticing isn’t enough. Taking timely action is essential for long-term health. This is why having a trusted General Physician in Delhi is not just a luxury but a necessity. From toddlers battling seasonal infections to grandparents managing chronic conditions, a reliable doctor can form the backbone of a family’s healthcare.
In a bustling city like Delhi—where seasons shift rapidly, pollution fluctuates, and stress is woven into daily life—maintaining health throughout the year requires consistency and foresight, not guesswork.
Why Every Family Needs a Go-To Doctor
The landscape of modern healthcare can be confusing and fragmented. With different doctors assigned for various problems and a plethora of opinions swirling around, the journey to health can feel overwhelming. A General Physician serves as a crucial touchpoint, simplifying this complexity. Whether it’s fever, fatigue, digestive issues, or unexplained symptoms, having one doctor to consult first leads to clearer decisions and effective care.
Families with a regular physician can approach health challenges with confidence rather than panic.

The True Value of a Family General Physician
A family doctor does more than just treat individual ailments; they recognize patterns within the family unit. When multiple family members fall ill at once or display similar symptoms, a General Physician often identifies potential environmental, lifestyle, or genetic factors that could be at play. For instance, if seasonal allergies affect several family members, a skilled physician can provide preventive care and actionable advice before problems escalate.
One such trusted name is Dr. Sanchayan Roy, who emphasizes preventive care, clear guidance, and a patient-centered approach.
Meet Dr. Sanchayan Roy: A Compassionate Healthcare Partner
Dr. Sanchayan Roy is well-regarded for his calm demeanor and approachable manner. He creates an atmosphere where patients feel neither rushed nor judged; they feel heard and respected. Dr. Roy’s dedication to understanding a patient’s medical history and lifestyle choices allows for tailored treatment plans. This continuity of care is invaluable, as it leads to more effective outcomes.
Serving Diverse Needs: From Children to Seniors
Children are prone to infections, adults may ignore symptoms due to work pressure, and seniors often juggle multiple health conditions. A General Physician in South Delhi, like Dr. Roy, effectively coordinates care across all age groups, ensuring that treatments make sense and that medication is not over-prescribed.
This balance plays a crucial role in preventing unnecessary visits to specialists and alleviating the burden on both the patient and the healthcare system.
Navigating Seasonal Illnesses and Daily Health
The changing seasons in Delhi can lead to health challenges such as viral fevers, allergies, and respiratory issues. A proactive General Physician prepares families in advance with actionable advice for prevention rather than solely relying on prescriptions after symptoms appear. This foresight can significantly improve the quality of life for families.
Addressing Breathing Issues: The Role of a General Physician
It’s common for families to seek out “Asthma Doctor Near Me” only after experiencing repeated episodes of coughing or wheezing. Many don’t realize that a General Physician is often the best initial contact. They can assess triggers like airborne allergens or pollution, offer immediate management strategies, and refer patients to specialists only when necessary.
Preventive Care That Saves Time and Reduces Anxiety
Routine checkups can catch hidden health issues—like high blood pressure, low immunity, or early signs of diabetes—before they escalate into emergencies. A committed General Physician in Delhi can help establish a foundation for better health and reduce the anxiety that comes with surprises.
Building Trust Through Clear Conversations
Transparent communication is crucial in healthcare, especially for families. A General Physician who explains medical concepts in simple terms fosters trust and helps parents make informed decisions, while also making seniors feel secure and not overwhelmed.
The Importance of Continuity of Care
There’s true power in seeing the same General Physician over the years. This relationship helps create a cohesive health narrative rather than a collection of disjointed medical reports. Trends become easier to identify, treatments are tailored more intelligently, and families can feel supported in their healthcare decisions.
The Doctor Every Family Needs
Health isn’t just about emergency visits; it’s about having the right doctor to turn to before a crisis strikes. With consistent guidance, practical advice, and genuine care, a General Physician in Delhi becomes an integral part of family wellbeing. Dr. Sanchayan Roy provides comprehensive family healthcare and preventive care, ensuring that no aspect of wellbeing is overlooked.
Conclusion: A Partnership for Lifelong Health
Families flourish when their healthcare feels familiar and reliable. From managing childhood fevers to addressing stress-related issues and breathing difficulties—having one trusted doctor is invaluable. Dr. Sanchayan Roy exemplifies the qualities every family deserves in a healthcare partner: a compassionate medical professional dedicated to caring for the entire family—not just isolated symptoms.
With extensive experience, Dr. Roy is recognized for his patient-first approach and his strong clinical acumen. Renowned as one of the best Pulmonologists in Delhi, he specializes in asthma, COPD, chronic cough, and allergies. He believes that effective treatment starts with understanding, taking the time to listen, and crafting personalized treatment plans that consider both symptoms and lifestyle.
Alongside his expertise in respiratory care, Dr. Sanchayan Roy also practices as a General Physician in Delhi, offering a holistic approach to healthcare. For common ailments such as fever, infections, diabetes management, and routine health concerns, he provides comprehensive guidance under one roof, ensuring that families receive the complete care they deserve.
Care
Understanding Your Cycle: Benefits of At-Home Ovulation Testing
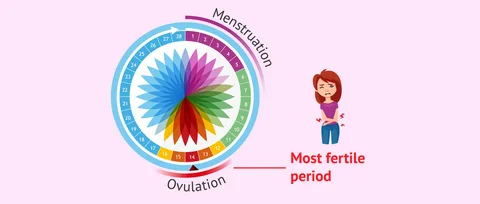
Most women find tracking ovulation tricky due to too many apps, graphs, or clinic visits. Yet knowing when it happens matters whether planning a baby, preventing one, or just being curious about how the body works. A straightforward test you can do at home cuts through the noise. Instead of guessing, there’s now a calm method right on your bathroom counter. That moment each month becomes less mysterious and clearer.
At home, testing means less stress and fewer trips to clinics because tracking happens where life already unfolds. Day by day, results build a picture of what’s normal, simply through routine moments adding up over time.
Easy At-Home Ovulation Test Explained?
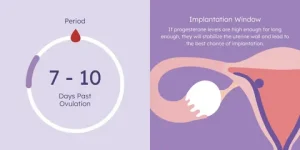
A little device used at home can spot when you’re close to ovulating. Because it picks up shifts in natural body chemicals linked to your monthly rhythm. Right before releasing an egg, there’s a rise in a hormone called luteinizing hormone. This spike tells the ovaries it is nearly time to let go of an egg.
A shift in hormones shows up in pee, so tracking helps spot the best time to get pregnant. By checking now and then, cycles make more sense, revealing exactly when chances rise sharply.
Tracking Ovulation Helps Understand Fertility Timing
Ovulation tracking gives women clearer insight into their bodies. Mood shifts, hunger levels, energy, and emotions often tie closely to hormone patterns. When the timing of ovulation is clear, it becomes easier to shape workouts, meals, schedules, and moments for self-care around what feels right.
Finding the right moment when trying to have a baby? Knowing which days are most fertile helps without extra effort. When preventing pregnancy, instead of keeping track of ovulation, backs up non-hormonal choices. Either way around, a simple test you take at home brings clearer answers.
How a Simple At-Home Ovulation Test Works
A shift in hormones shows up in pee just before an egg is released. As those chemicals climb, the strip picks it up with a clear sign. Most of the time, this happens a day or so before ovulation, giving extra time to prepare.
A handful of days ahead of expected ovulation, most women begin checking each morning. As weeks pass, subtle clues emerge, linking together in ways unique to their bodies. Testing becomes routine, day after day, until the shift shows up on the strip.
Easy At-Home Ovulation Test Benefits
What stands out most is how easy it gets. Doing the test inside your place just slips into whatever you already do each morning. There are no scheduled slots to keep, no trips to clinics, and nothing bulky or confusing to set up. Answers show up fast, so there is no pause in your usual flow. The whole thing moves quietly alongside life.
Finding privacy matters a lot to some people. For many women, watching their cycle feels too private for outside eyes. Conducting tests within their own space allows them to progress through each step without drawing attention. Comfort comes easier when no one else is involved.
When things stay routine, it gets simpler. Because the method isn’t complicated, many women tend to check often this builds a clearer picture of their cycle as weeks pass.
Make testing part of daily life
Some women go for a morning check, yet a few pick late hours based on how their day rolls. The key thing? Staying steady. Doing it at the same hour every time brings sharper results into view.
A few cycles in, many notice their ovulation settling into a pattern. Because of this shift, checking each day starts to seem less like work and just part of the flow.
Staying Calm While Reviewing Test Outcomes
First thing you notice might be the mess of numbers. One day blurs into the next, and then suddenly a spike appears. Watch the flow across mornings and evenings rather than fixating on any single mark.
Later on, spotting familiar signs feels more natural. As women discover what their bodies typically do, assurance grows. With that quiet knowing comes less worry and a steadier faith in how tests work.
Things that might change ovulation test outcomes
Tiny shifts happen when life gets busy. Hormone levels react to how you live each day. When stress piles up, everything inside tweaks a bit. Ovulation might move ahead or lag if rest feels scarce. Not drinking enough water plays its part, too. A cold or long trip nudges things off rhythm. The body adjusts without alarm. Tests still work just fine through those small wobbles. Nothing breaks because of ordinary hiccups.
A shift in daily habits can shape how the body behaves, making calm persistence easier for many women. When you watch several monthly cycles unfold, trends begin to stand out, revealing what’s typical for one person.
Feeling at ease with home testing
Finding balance can be tough when trying to conceive, particularly with hormones shifting unpredictably. A straightforward test used privately brings ease, replacing stress with quiet confidence during personal moments.
Out there, away from eyes and clocks, testing becomes something a woman can shape on her own terms. Because of that quiet space, staying with it week after week feels less like effort. Cycle patterns begin to make more sense when seen through a steady, personal rhythm.
People tracking ovulation at home with easy tests?
Starting slow works well for women drawn to minimal effort. Because clarity matters, this approach skips tangled instructions. Those new to monitoring fertility tend to land here first; its rhythm teaches without pressure.
Over time, those tracking each day might start noticing shifts, especially when periods don’t come like clockwork. A different rhythm reveals itself only after several months of watching closely.
Dr. Alan Lindemann, Trusted Fertility & Saliva Ovulation Expert at KNOWHEN
Dr. Alan Lindemann, an experienced obstetrician with nearly four decades of practice and over 6,000 safe deliveries, provides trusted guidance on using the KNOWHEN® saliva ovulation test to track fertile days naturally. He empowers women with expert reproductive health insight, highlighting how this simple, non-invasive, and reusable method makes fertility awareness easier and more confident without clinic visits or complicated procedures. His expert advice supports informed decisions about ovulation timing, cycle understanding, and natural family planning.
In this blog, Dr. Alan shares clear insights on how home ovulation tests help women track fertile days easily and privately. He explains how simple at-home testing detects natural hormonal changes to identify ovulation without clinic visits. Ideal for fertility awareness, cycle understanding, pregnancy planning, or natural birth control, this guide highlights a calm, reliable, and stress-free approach to understanding your body at home.
At-Home Ovulation Tests Compared to Other Approaches
Tracking fertility happens in different ways. Some pick calendars; others check body heat daily instead. Medical tests give data, too. In between watching signs naturally and lab work, there is a middle path. That spot belongs to simple ovulation kits used at home. These tools fit quietly into routines. Information shows up clearly without doctor visits. Not every approach works the same for everyone. Personal rhythm matters most when trying to understand timing.
Fresh data on hormones shows up instantly; no doctor trips needed. Some pair those results with notes on their monthly patterns along with physical cues, building clearer pictures of when they might conceive.
Tracking Ovulation Changes Across Time
Month by month, watching for ovulation gives women clearer insight into how their cycle works. Suddenly, shifts in energy levels, emotions, or body signals feel less confusing. With that clarity comes a stronger sense of balance and more space to listen to what the body needs.
Each day of checking brings you closer to how your body works. Slowly, knowing about fertility fits into daily life without pressure.
Conclusion
Home ovulation tests make spotting fertile times straightforward, minus the stress. Hormone shifts give clear signs when checked each day privately. Comfort grows from routine testing, away from clinics or judgment. Personal timing becomes clearer through steady observation, nothing more.
A clearer understanding of fertility often develops slowly, through consistent effort over time. Ovulation can make sense without confusion or stress. Small routines each day might reveal what matters most.
FAQs
Can an easy at-home ovulation test be used with irregular cycles?
Frequently, spotting trends takes longer when periods are unpredictable. Yet sticking with regular checks usually shows useful clues eventually.
Is it normal to see different results each month?
Of course. Body chemistry adjusts on its own when daily habits shift, stress piles up, rest drops off, or wellness dips, throwing cycle cues out of sync.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom