Uncategorized
Reviewing Your Options in Light of Recent Cancer Treatment Advances
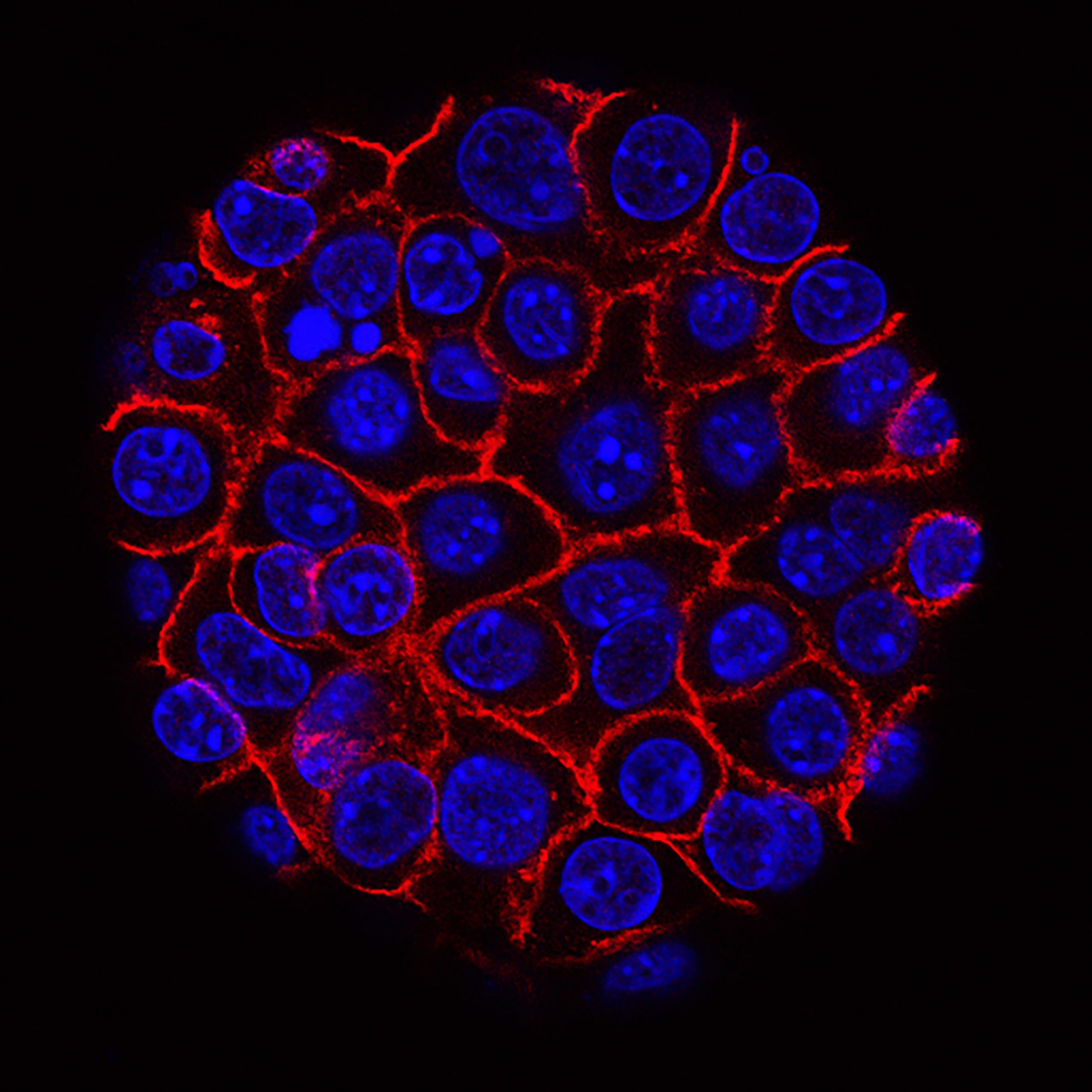
A cancer diagnosis can be distressing, but there is reason for hope thanks to advances in science and medicine. Numerous cancer survivors’ stories highlight the value of a well-thought-out treatment program. As novel cancer treatments are being developed at a rapid rate, patients today have more choices than ever before. Immunotherapy and other targeted pharmaceutical medications may be part of these treatments, which could result in remission or perhaps a cure. Here, we’ll examine the current landscape of cancer treatment options and have an open conversation about how they could be used to help people cope with and ultimately overcome this awful disease.
Surgery
It’s important to remember that there are many different surgical options for treating cancer. The optimal surgical strategy for each given patient depends on a number of criteria, including the type and stage of the cancer, the patient’s overall condition, and the surgeon’s level of experience.
The following are some of the more common surgical procedures performed for cancer patients.
A lumpectomy is surgery to remove a breast tumor. This method is also known as a “partial mastectomy.” Lumpectomy is a common surgical treatment for treating breast cancer in its early stages.
A mastectomy is the surgical removal of both of a woman’s breasts. A mastectomy is an option for women with advanced breast cancer.
Surgery to remove the prostate gland is called a prostatectomy. A prostatectomy is commonly prescribed for men who have been diagnosed with prostate cancer at an early stage.
Radiation therapy uses X-rays and other high-energy radiation sources to eradicate cancer cells. Both external radiation therapy devices and radioactive materials implanted at or near the tumor are viable options for delivering radiation therapy.
Chemotherapy
Chemotherapy refers to the use of drugs in the treatment of cancer. Chemotherapy is not limited to intravenous (IV) use; it can either be ingested or applied topically (as a cream or ointment). It is often delivered in cycles, with each cycle including both a treatment period and a recovery phase. It is usual practice to combine chemotherapy with other treatments.
Weakness, nausea, vomiting, hair loss, mouth sores, and a heightened susceptibility to infection are just some of the unpleasant side effects of chemotherapy. Some people may develop extremely serious adverse effects, such as organ failure or an allergic reaction.
Chemotherapy is not appropriate for all patients with cancer. Your doctor will think carefully about your overall health, the specifics of your disease, and the results you want to achieve before recommending chemotherapy as a treatment.
Radiosurgery
In order to eradicate malignant tissue, radiosurgery is used as a treatment option. The radiation therapy only affects the tumor, sparing the surrounding healthy tissue. Therefore, radiosurgery is highly effective for patients with low-grade, locally-confined cancers.
Radiosurgical patients can often return home the same day they were treated. A typical day can be resumed after less than an hour of downtime is required. The time needed to recuperate could range from a few days to a few weeks, depending on the size and location of the tumor.
Dr. Gil Lederman heads up a top-notch New York cancer radiosurgery center.
Immunotherapy
Immunotherapy’s success in human studies as a fresh approach to cancer treatment is exciting. With immunotherapy, a patient’s immune system is boosted in an effort to speed up the natural death rate of cancer cells. There are a number of immunotherapies available, and they each have their own unique mechanism of action.
Using checkpoint inhibitors, immunotherapists disable proteins that act as immune system brakes. The immune system’s capacity to recognize cancer cells and destroy them is thereby enhanced. Checkpoint inhibitors have shown promise in the treatment of melanoma and lung cancer, and their utility in combating other cancers is also being investigated.
In adoptive cell therapy, the patient’s own immune cells are employed after being separated and modified in the lab to be more effective against cancer cells. The modified cells are reintroduced to the patient so that their immune system can better combat cancer. The effectiveness of adoptive cell therapy in the treatment of various cancers is now being investigated in clinical trials.
Immunotherapy is a relatively new area of cancer study with enormous potential to improve patients’ outcomes.
Care That Is Specifically Intended
The purpose of targeted therapy in the treatment of cancer is to block the activity of one or more individual chemicals or genes that promote tumor growth and spread. It is usual practice to combine this therapy with other cancer treatments. Targeted therapy has the potential to kill cancer cells more effectively while minimizing damage to healthy tissue.
Human Subjects Experimentation in the Health Sciences
Patients with cancer now have many therapeutic options thanks to clinical trials. The general public needs to be aware that novel cancer treatments are being tried in clinical trials.
Clinical trials, like any other scientific endeavor, can have a wide range of aims, time frames, and organizational structures. While other clinical trials investigate novel treatments that have not yet been made available to the public, others examine tried-and-true methods for the first time in regard to a specific cancer or group of cancers. Clinical trials are a useful tool for evaluating new approaches to cancer prevention, screening, and diagnosis.
Clinical trials are conducted by researchers in a wide variety of settings, from academic medical centers and government research institutes to private practices and community health clinics. It may take quite some time after a medicine has undergone extensive testing in the lab before it is ready to be tested on human volunteers in a clinical study.
If you’re a cancer patient contemplating about taking part in a trial, you and your doctor should talk about the pros and cons. Clinical trials aren’t always the most effective path of treatment because each patient’s disease is unique. Nonetheless, clinical trials are some patients’ greatest bet for receiving a successful medicine.
Assistance Provided
Cancer patients have access to a wide variety of treatment options, and determining which one would be most successful for them requires consideration of their individual needs. But supportive care, which attempts to reduce symptoms associated with cancer and its treatment, is beneficial for everyone who has the condition.
As part of a bigger network of care, services like pain management, nutritional advice, and emotional support can be offered. In order to get the best possible supportive care, cancer patients should work with a healthcare team that is experienced with their illness.
Those dealing with cancer often experience depression and anxiety. They can receive supportive care to help them cope with these challenges and improve their quality of life overall.
Identifying Your Specific Treatment and Intervention Needs and Learning to Implement Them
Cancer treatment options have improved greatly in recent years. It may be difficult to determine the best course of action to take in your situation. As you weigh your treatment options, keep in mind the following:
In any case, why are we making an attempt to treat it?
Patients with cancer may eventually have to accept illness management as an acceptable alternative to a cure. To what extent you answer this question honestly will help establish the best therapeutic approach to take with you.
Please tell me how dangerous this treatment is.
There may be some unwanted side effects with every treatment you choose. Symptoms might range from annoying to life-threatening. Think about the potential adverse reactions the treatment could cause.
The most pressing question is how long will I have to go through this therapy.
Treatments can be utilized in either a short-term or long-term capacity. Consider how much time you can realistically dedicate to treatment before beginning.
Do you have any idea how much money would be needed for something like this to be done in a hospital?
The cost of cancer treatment can quickly add up. Before deciding to pursue therapy, one should assess their financial circumstances.
Conclusion
As a result, there are now many more cancer treatments available to people today. Developing a treatment plan for a patient requires consideration of their unique requirements (which may include anything from surgery and chemotherapy to radiation and immunotherapy to targeted drugs). You should know what kinds of treatments are out there so you can pick the one that’s ideal for you. If you feel you need help, it’s important to talk to your doctor or health care team, who may provide personalized recommendations for you depending on your condition and other considerations.
Business
Unity 3D Game Development in 2025: First Choice for Scalable

Quick Answer: Unity 3D game development leverages the Unity engine to create visually rich, scalable, and cross-platform games. It supports 3D rendering, AR/VR integrations, multiplayer features, and real-time simulation. In 2025, Unity remains the go-to choice for startups and enterprises alike to build immersive games for mobile, PC, console, and the metaverse.
What is Unity 3D Game Development?
Unity 3D game development is the process of using the Unity game engine to build three-dimensional games. It allows developers to:
- Build interactive environments
- Animate 3D characters
- Apply physics simulations
- Integrate real-time lighting and shading
- Deploy to Android, iOS, Windows, consoles, AR, and VR
Unity uses C# scripting, making it ideal for both indie developers and enterprise-grade studios. Learn more about our Game Development Company
Why Unity Is Still the Top Game Engine in 2025
Unity leads because of its flexibility and toolset:
- Cross-platform deployment (25+ platforms including consoles and WebGL)
- Robust Asset Store with prebuilt 3D models and systems
- AR/VR toolkit with native support for Oculus, Vision Pro, HoloLens
- Unity DOTS & ECS (for performance-based coding)
- Unity Cloud Build and CI/CD integrations
In a 2025 developer survey, 61% preferred Unity for 3D games due to its quick learning curve and scalability.

Considering Unity vs Unreal? Ask our experts which suits your goals
Top Use Cases for Unity 3D Games
Unity powers a wide variety of 3D game genres:
- First-person shooters (FPS)
- Adventure & platformer games
- Survival & sandbox simulators
- Racing and sports titles
- Multiplayer co-op or PvP games
- Metaverse exploration environments
Businesses also use Unity for training simulations, education apps, and brand gamification. See how our AR Game Development Company brings Unity into immersive AR projects.
Core Benefits of Unity 3D for Developers & Businesses
FeatureBenefitCross-Platform BuildLaunch your game on iOS, Android, Windows, consolesReal-Time RenderingCinematic visuals at runtimeAsset Store AccessSpeed up development with ready-to-use assetsMultiplayer FrameworksBuilt-in support for Photon, Netcode, MirrorIn-App MonetizationUnity Ads, IAP, subscriptions, in-game economiesScalabilityEasily scale servers and performance with Unity Cloud
Our Unity 3D Game Development Process
At Vasundhara, we follow a tested Unity 3D development lifecycle:
- Concept Planning & Wireframes
- Asset Planning & 3D Design
- Gameplay Logic with C# + Unity Editor
- AR/VR or Multiplayer Integration
- Performance Tuning + Bug Testing
- App Store Deployment + SDK integrations
- LiveOps: Analytics, Patches, Leaderboards
Learn more about our Mobile App Development Services
Key Tools & Technologies Used in Unity Projects
We use advanced tech to supercharge our Unity projects:
- Unity Pro / Unity Enterprise licenses
- Photon Engine / Netcode for Multiplayer
- Blender & Maya for 3D asset design
- Unity MARS for AR game interactions
- Unity Performance Profiler
- Unity Remote Config + Unity Analytics
Our stack ensures games are fast, bug-free, and scalable.
Real-World Projects Built With Unity
From global hits to indie successes, Unity powers:
- Among Us (multiplayer logic)
- Monument Valley (3D puzzle)
- Beat Saber (VR integration)
- Pokemon Go (AR layer)
At Vasundhara, we’ve delivered Unity games for:
- Simulation training (enterprise)
- Mobile RPGs (freemium models)
- Augmented reality adventures
Why Choose Vasundhara as Your Unity 3D Game Partner
✅ 12+ Years in Game Development (Unity Certified Engineers) ✅ 250+ Projects Delivered Globally ✅ Unity Pro License & Photon Experts ✅ Scalable CI/CD Deployment Pipeline ✅ Real-time Optimization for 60+ FPS Games
We align with your vision, budget, and target audience.
Explore our custom software development services that complement Unity games with backend services.
Ready to build a high-performance Unity 3D game? Contact our team now
Conclusion:
Unity 3D game development empowers creators to build immersive, scalable, and revenue-ready games across any platform. In 2025, businesses and developers trust Vasundhara Infotech for custom 3D Unity games with multiplayer, AR/VR, and metaverse-ready capabilities.
Have a Unity 3D game idea? Let’s turn it into reality
FAQs — Unity 3D Game Development, Vasundhara Infotech
1. Is Unity worth using in 2025?
Yes, Unity remains a highly relevant and powerful game development engine in 2025. Its continuous updates, strong community, extensive asset store, and support for AR/VR, mobile, console, and PC make it a great choice for both indie and professional developers. Unity’s flexible licensing and low barrier to entry also keep it appealing to beginners and small studios.
2. Does Unity support cross-platform development?
Absolutely. Unity is designed with cross-platform compatibility in mind. You can build your game once and deploy it to over 20 platforms, including Windows, macOS, iOS, Android, PlayStation, Xbox, Nintendo Switch, WebGL, and more — all with minimal changes to your code.
3. What is the Unity controversy?
The “Unity controversy” typically refers to the backlash in late 2023 when Unity announced changes to its pricing model, introducing a new “Runtime Fee” based on game installs. Many developers criticized the lack of transparency and the potential financial impact on smaller studios. Unity later revised its policies in response to community feedback, but the episode highlighted the importance of clear and fair business practices in the industry.
4. How does Unity handle multi-platform game development?
Unity uses an abstraction layer and platform-specific build settings to make multi-platform development seamless. Developers write most of their code in C# once, while Unity’s editor and build pipeline handle the differences in rendering, input, and deployment for each platform. You can also use conditional compilation and platform-specific APIs when needed.
5. What is the best platform for game development?
There is no single “best” platform; it depends on your goals:
- For beginners and indies, Unity is one of the best due to ease of use, cross-platform support, and community resources.
- For high-end AAA graphics, Unreal Engine might be better suited.
- For 2D games, both Unity and tools like Godot are excellent.
- For web and casual games, HTML5 frameworks or Unity WebGL can work well.
Need help choosing a platform? Contact Vasundhara Infotech for the target devices and your project’s technical needs.
Game
Is It Time for Skulls Ludo’s $SKL Token to Go Cross-Chain?
The blockchain gaming landscape is evolving—fast. As players demand faster transactions, lower gas fees, and broader accessibility, the infrastructure behind GameFi must evolve too. Skulls Ludo, a rapidly rising play-to-earn Ludo NFT game, has already made waves by building on Polygon, leveraging its speed and scalability. But the next frontier might not lie within one chain—it lies across many.
In a world where Solana NFT games, BNB Chain dApps, and Ethereum-based collectibles co-exist, the idea of a multi-chain gaming economy is no longer theoretical—it’s essential. This brings us to an exciting, forward-looking question:
Could Skulls Ludo’s $SKL token expand beyond Polygon—and what would that mean for players, investors, and the future of blockchain gaming?
Why Was Skulls Ludo Built on Polygon in the First Place?
Before we explore expansion, it’s crucial to understand the strategic choice of Polygon as Skulls Ludo’s home.
Key reasons Polygon was chosen:
- Low Transaction Fees: A fraction of a cent per transaction enables micro-transactions for in-game rewards and NFT purchases.
- High Throughput: Supports thousands of transactions per second—crucial for real-time multiplayer gameplay.
- Ethereum Compatibility: Seamless interoperability with Ethereum tools, wallets, and marketplaces.
- Eco-Friendly: A more sustainable option compared to Ethereum’s earlier energy-intensive operations.
Polygon has provided a solid foundation for $SKL tokenomics, gameplay logic, and NFT trading. But as Skulls Ludo scales, so do the needs and ambitions of its ecosystem.
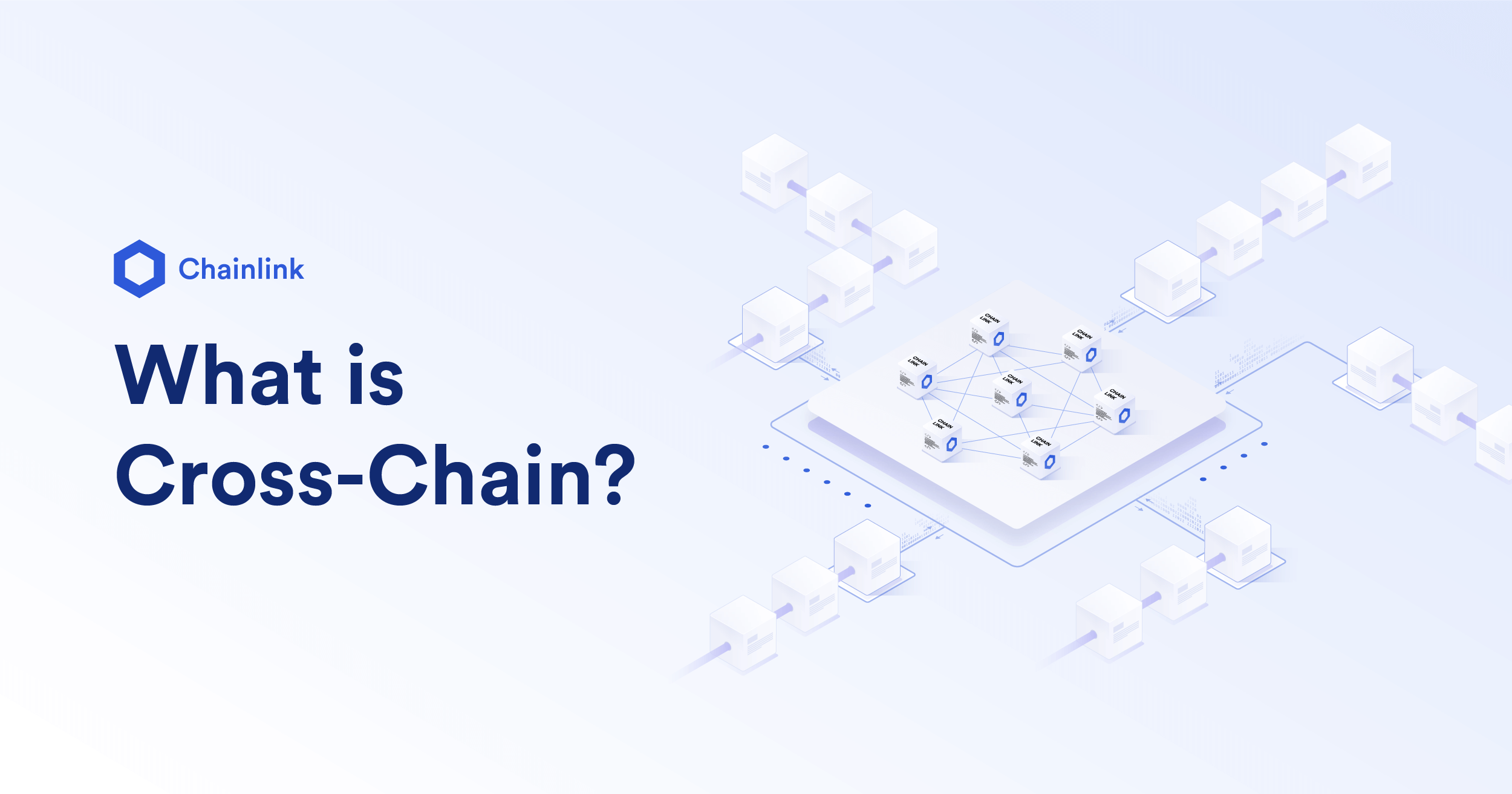
What Is a Multi-Chain Gaming Economy—and Why Does It Matter?
A multi-chain gaming economy refers to the ability of a GameFi ecosystem to operate across multiple blockchain networks simultaneously. Rather than being siloed into one chain, assets like tokens, NFTs, and game logic can move, interact, and be recognized across chains like Ethereum, Solana, Avalanche, and BNB Chain.
Why does this matter?
- Greater Liquidity: Multiple exchanges, bridges, and liquidity pools increase token accessibility.
- Broader User Base: Tap into new communities on Solana, BNB Chain, and Layer-2s.
- Developer Flexibility: Build features optimized for each chain’s strengths.
- Cross-Chain NFTs: Enable NFTs to be moved or recognized across ecosystems.
- Network Resilience: Avoid bottlenecks or outages on a single chain.
For Skulls Ludo, going multi-chain means unlocking new crypto gaming platforms, appealing to a larger player base, and future-proofing the project in an increasingly interoperable Web3 world.
What Would Multi-Chain Expansion Look Like for $SKL?
Let’s break this down practically. How would $SKL function in a multi-chain world?
Scenario 1: Cross-Chain Token Bridging
- $SKL can be bridged to other chains (e.g., Solana, BNB, Base) via smart contracts and wrapped tokens.
- Players on these chains can earn, stake, and trade $SKL without leaving their native wallets or environments.
Scenario 2: Chain-Specific Gameplay Zones
- Unique game modes or tournaments are launched on separate chains (e.g., “Solana Arena” or “BNB Showdown”) powered by bridged $SKL.
- Encourages network-specific communities to engage and compete.
Scenario 3: Interoperable NFTs
- Ludo game NFTs can be mirrored or moved between chains using cross-chain NFT standards like LayerZero, Wormhole, or Axelar.
- This allows trading across OpenSea (Polygon), Magic Eden (Solana), and more.
Scenario 4: Unified Treasury & Governance
- No matter which chain you’re on, $SKL holders can participate in unified DAO governance, stake across chains, and influence future development.
Benefits of Going Multi-Chain for Skulls Ludo Players and Investors
For Players:
- Play from any chain without having to migrate wallets.
- Compete in tournaments with a global player pool.
- Access exclusive in-game items or NFTs specific to a chain.
For NFT Collectors:
- Trade NFTs across multiple marketplaces for better liquidity.
- Interact with evolving GameFi ecosystems (like Solana’s compressed NFTs or Avalanche subnets).
For Investors:
- Increased token visibility and adoption across chains boosts $SKL demand.
- More staking options and DeFi integrations.
- Diversified liquidity reduces systemic risk of any single chain failure.
Why Solana, BNB Chain, or Avalanche Could Be Strategic for $SKL
Solana
- High-speed, low-cost.
- Vibrant NFT ecosystem with marketplaces like Magic Eden.
- Strong GameFi developer tools (ex: Metaplex, Anchor).
BNB Chain
- Massive retail user base in Asia.
- Easy CEX listings for liquidity.
- BNB gaming guilds and influencer networks.
Avalanche / Subnets
- Custom game-optimized chains.
- Better control over scalability and resource allocation.
- Low-latency gameplay support.
What Are the Risks or Challenges of Going Multi-Chain?
While the upside is clear, multi-chain expansion isn’t plug-and-play.
Key challenges:
- Technical Complexity: Bridging smart contracts can be exploited if not audited properly.
- Fragmentation Risk: Splitting the user base without careful UX design can cause confusion.
- Liquidity Spread: Dividing token supply across chains could affect price stability.
- Security Risks: Cross-chain bridges have historically been vulnerable (see: Wormhole, Harmony hacks).
Skulls Ludo must balance innovation with stability, ensuring each expansion is strategically timed and community-backed.
Is the Community Ready for a Multi-Chain Skulls Ludo?
Before going cross-chain, the real question is: does the community want it?
This is where DAO governance plays a critical role. $SKL holders could:
- Vote on which chain to expand to first.
- Decide on token allocations for liquidity pools.
- Propose game features exclusive to new chains.
A multi-chain world must be built with the community—not just for it.
The Multi-Chain Future Starts with $SKL’s Vision
Blockchain gaming isn’t about just building games—it’s about building economies that move, evolve, and scale with their communities. Skulls Ludo’s potential to become a multi-chain GameFi powerhouse rests on the strength of its $SKL token, the scalability of its platform, and the vision to go where the players are.
By exploring multi-chain expansion, Skulls Ludo can:
- Onboard thousands of new players from different ecosystems.
- Offer flexible, resilient gameplay infrastructure.
- Strengthen the long-term utility and value of $SKL.
If GameFi is the next frontier of gaming, then multi-chain economies are the infrastructure that powers it—and Skulls Ludo is already rolling the dice.
Uncategorized
Women in Tech: Certifications That Are Opening Doors in 2025
-
Business2 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business2 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business2 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health2 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports2 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment2 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance2 years ago
The Benefits of Starting a Side Hustle for Financial Freedom































