health
From Combat to Coverage: How These Female Veterans Struggled for Proper Health Care

As women, we’re often told that we can do anything. And for many of us, serving in the military is a dream come true – an opportunity to defend our country with honor and distinction. But what happens when that service ends, and you find yourself struggling to receive the medical care you need? For many female veterans, this all-too-common struggle has become a harsh reality. In this blog post, we’ll explore the stories of several brave women who have fought tooth and nail for proper health care after their time in combat ended. Their stories are inspiring, heart-wrenching, and above all else – necessary listening for anyone who cares about our veterans’ well-being.
The Struggle to Access Health Care
In 2007, shortly after completing her combat deployment in Iraq, Army National Guard veteran Tabitha Cruse began experiencing debilitating panic attacks. Struggling to cope with the physical and emotional aftermath of war, Cruse was unable to access the care she needed to get relief from her symptoms.
“The VA [Veterans Administration] didn’t really have anything for post-traumatic stress disorder,” Cruse said. “They just gave me some medication and told me that I should go see a therapist.”
For years following her deployment, Cruse struggled to find the resources she needed to address the debilitating panic attacks that had plagued her since returning from Iraq. After multiple visits to Veterans Affairs hospitals and appointments with mental health professionals, Cruse was only partially successful in finding relief from her symptoms. Finally, in 2013, after seeking treatment for chronic fatigue syndrome (CFS) for more than two years, Cruse was diagnosed with PTSD and CFS by a new doctor at a specialized clinic.
Since being diagnosed with PTSD and CFS, Cruse has received extensive care from both specialists and primary care doctors who have been able to provide her with much-needed relief from her debilitating symptoms. However, despite receiving appropriate care for her conditions, many female veterans like Tabitha Cruse remain severely underserved when it comes to accessing quality health care.
According to a study released by the Department of Veterans Affairs in 2014,[1] approximately 27 percent of female veterans are
The Lack of Resources and Support
Combat Veterans often experience Post Traumatic Stress Disorder (PTSD) and other emotional issues that can prevent them from finding or maintaining a job. For many female veterans, the struggles to find adequate health care are even more intense. Studies show that women experience PTSD at a rate of twice as much as men,[1] and therefore have an increased need for mental health services. This is particularly true for female veterans who have served in combat roles.
Many female veterans have difficulty accessing VA health care due to the fact that they are not regularly included in decision-making processes about Veteran’s Affairs programs and services. These veterans also face discrimination from doctors, nurses, and other healthcare providers when trying to seek help for PTSD or other medical conditions. In some cases, these women have been refused treatment outright or been forced to wait weeks or even months for an appointment. As a result, many female veterans resort to self-medication with alcohol or drugs in order to cope with their difficulties.[2]
It is essential that the VA provide more effective and accessible mental health care services for all combat veterans, regardless of gender. The VA should also work harder to include female veterans in decision-making processes about Veteran’s Affairs programs and services so that they can receive the support they need to rebuild their lives after serving their country.
The Denial of Treatment
Since the end of the Vietnam War, military women have been fighting for equal treatment and health care. Despite decades of progress, many female veterans still experience discrimination when seeking medical care.
Women in the military are regularly exposed to toxic substances, including Agent Orange and landmines. This often leads to chronic health conditions such as post-traumatic stress disorder (PTSD) and substance abuse. In addition, female veterans are more likely than men to suffer from sexual assault or domestic violence while serving in the Armed Forces.
As a result of these experiences, many female veterans struggle with mental health issues and physical injuries that go untreated. These conditions can lead to long-term disability, which is why it’s so important that they receive proper medical care.
Unfortunately, many female veterans don’t have access to quality healthcare due to discrimination and outdated policies. For example, women often face barriers when trying to get pregnant while in the military or receiving fertility treatments after leaving service. This leaves these veteran women at a disadvantage when it comes to accessing quality healthcare resources.
It’s critical that we continue working hard to improve the quality of healthcare for female veterans. We must make sure that they’ve access to all the necessary resources so that they can heal from their traumatic experiences and move on with their lives
Discrimination and Harassment
Female veterans have long been marginalized within the U.S. military and society at large, often facing discrimination and harassment. This has led to inadequate health care and other services, compounded by a lack of knowledge about veteran’s rights and benefits.
Many female veterans have suffered from poor mental health as a result of their experiences in the military, which can further complicate their access to quality care. Additionally, many women have experienced sexual assault while serving in the armed forces, which can lead to lasting trauma and PTSD.
Despite these obstacles, many female veterans are working hard to get the care they need and deserve. In order to improve healthcare for all veteran populations, it is important that we learn about the unique challenges faced by female veterans and work together to create solutions.
The Military’s Role in the Health Care System
The military has long been seen as a cornerstone of the health care system in the United States. This is largely due to the fact that the military provides essential health care for its members, regardless of their location or socioeconomic status. In recent years, however, there has been a growing concern over how well the military’s role in the health care system corresponds with actual needs.
Female veterans are no exception to this trend. According to one study, female veterans face unique challenges when it comes to accessing appropriate health care due to their combat experiences. Female veterans are more likely than male veterans to experience post-traumatic stress disorder (PTSD) and other mental health issues. This can make it difficult for them to navigate the medical system, especially if they do not speak English fluently.
In order to address these challenges, many female veterans have turned to private healthcare providers or VA facilities. However, these options often do not meet their needs or cover all of their expenses. As a result, many female veterans have had to resort to using emergency rooms or seeking out free or low-cost care from hospitals and clinics outside of the military chain of command. These efforts can be expensive and time-consuming, leading some women to forgo necessary treatment altogether.
Overall, female veterans face significant obstacles when it comes to accessing quality health care. The Military Health System does not always meet their needs properly, while private healthcare providers and VA facilities often do not provide adequate coverage or services.
Conclusion
For many female veterans, seeking quality health care was a long and difficult process. Despite fighting for the same rights as their male counterparts, many women felt that they did not receive the same level of care when it came to accessing healthcare. This lack of access to proper healthcare can have far-reaching consequences for both mental and physical health, which is why it is so important that we work hard to ensure that all our veteran citizens are able to get the best possible treatment available.
health
Typhoid Fever: Causes, Symptoms And Treatment
Introduction
Typhoid fever is a serious infection that affects millions of people worldwide each year. Caused by the bacterium Salmonella typhi, typhoid spreads through contaminated food and water, especially in areas with poor sanitation. Early signs can be mild—a low-grade fever or headache—but without prompt treatment, the illness can lead to high fever, severe stomach pain, and life-threatening complications. In this guide, we’ll explain the causes of typhoid, how the infection spreads, the symptoms to watch for, and the most effective treatments available. By understanding these key points, you can protect yourself and your family from this preventable disease.
What Is Typhoid Fever?
Typhoid fever is a bacterial illness transmitted through ingestion of food or water contaminated with Salmonella typhi. Unlike common food poisoning, typhoid can invade the bloodstream and spread throughout the body. It remains a global health challenge, with the highest burden in South Asia and sub-Saharan Africa, but travelers to any region with poor water treatment can be at risk.
Causes of Typhoid Fever
The root cause of typhoid fever is the bacterium Salmonella enterica serotype Typhi. Key factors include:
- Contaminated Water: Drinking or cooking with water tainted by sewage containing S. typhi.
- Contaminated Food: Fruits, vegetables, and ready-to-eat foods washed or handled by infected individuals.
- Poor Sanitation: Lack of clean toilets and hand-washing facilities spreads bacteria.
- Carrier Transmission: Some recovered individuals carry S. typhi in their gallbladders and shed bacteria in stool for months or years.
How Typhoid Spreads
Understanding transmission helps with prevention. S. typhi spreads via the “fecal-oral route”:
- An infected person uses the bathroom and doesn’t wash hands properly.
- Bacteria remain on hands and transfer to food, water, or surfaces.
- Others consume the contaminated items and become infected.
Good hygiene and safe water practices break this cycle.
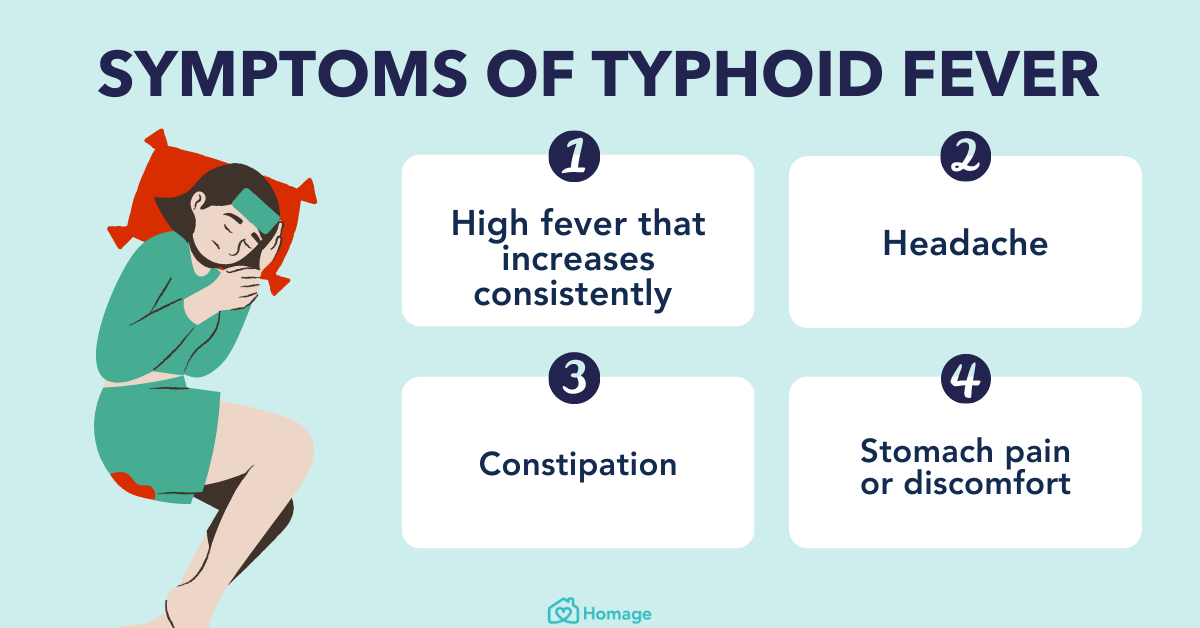
Symptoms of Typhoid Fever
Typhoid symptoms typically appear 6–30 days after exposure. They develop in stages:
- Week 1:
- Low-grade fever rising each day
- Headache and general weakness
- Abdominal discomfort
- Week 2:
- High fever (up to 104°F or 40°C)
- Persistent cough
- Rose-colored spots on chest or abdomen
- Severe stomach pain
- Week 3 and Beyond:
- Diarrhea or constipation
- Delirium, confusion, or severe weakness
- Intestinal bleeding or perforation (rare but serious)
Not everyone shows all signs. Children and elderly patients may have atypical symptoms like lethargy or lack of appetite.
Diagnosing Typhoid Fever
Early diagnosis speeds up treatment and reduces complications. Common tests include:
- Blood Culture: Detects S. typhi in the bloodstream—most accurate in the first week.
- Stool or Urine Culture: Used if blood cultures are negative or illness is prolonged.
- Widal Test: Measures antibodies against S. typhi but can give false positives, especially where typhoid is common.
Doctors also consider travel history, exposure risk, and symptom patterns.
Effective Treatment for Typhoid Fever
Prompt antibiotic treatment is crucial. Commonly prescribed medications:
- Ciprofloxacin or Ofloxacin: Shown effective in areas with low antibiotic resistance.
- Azithromycin: Preferred in regions where fluoroquinolone resistance is high.
- Third-Generation Cephalosporins (e.g., Ceftriaxone): Used for severe cases and intravenous therapy.
Supportive Care
- Hydration: Oral rehydration solutions replace lost fluids and electrolytes.
- Nutrition: Easy-to-digest foods—rice, bananas, and clear broths—aid recovery.
- Rest: Complete bed rest speeds healing and prevents complications.
Duration of Therapy
Treatment often lasts 7–14 days. Finish the full course even if symptoms improve to prevent relapse and resistance.
Preventing Typhoid Fever
Prevention combines vaccines, hygiene, and safe food practices:
1. Vaccination
- Oral Live-Attenuated Vaccine: Taken as four pills over one week; protective for 5–7 years.
- Injectable Capsular Polysaccharide Vaccine: Single shot; protection for ~2 years.
Vaccines are recommended for travelers to high-risk areas and close contacts of chronic carriers.
2. Safe Water and Food
- Drink bottled or boiled water; avoid ice in countries with unsafe water.
- Eat fully cooked foods served hot; avoid raw produce unless you peel it yourself.
- Wash hands thoroughly with soap and water before eating and after using the bathroom.
3. Personal Hygiene
- Wash hands for at least 20 seconds, especially after bathroom use.
- Use hand sanitizer (60% alcohol) when soap and water are unavailable.
- Maintain clean kitchen surfaces and utensils.
Risk Factors for Typhoid Fever
Certain groups face higher risk:
- Travelers: Especially to South Asia, Africa, and parts of Latin America.
- Healthcare Workers: Contact with infected patients or lab cultures.
- Those in Endemic Regions: Limited access to clean water and sanitation.
- Household Contacts: Family members of chronic carriers.
Awareness of risk factors guides targeted prevention measures.
Complications and When to Seek Emergency Care
Untreated typhoid can cause severe issues:
- Intestinal Perforation: Hole in the gut lining leading to life-threatening infection.
- Massive Gastrointestinal Bleeding: May require blood transfusion.
- Encephalopathy: Brain involvement leading to confusion or seizures.
- Sepsis: Widespread infection in the bloodstream.
Warning Signs
Seek immediate medical attention if you notice:
- Sudden severe belly pain
- Bloody or black, tarry stools
- High, unrelenting fever
- Extreme drowsiness or confusion
Early hospital care can prevent fatal outcomes.
Living with and Recovering from Typhoid
Most people recover fully with treatment but should follow these tips:
- Rest and Nutrition: Gradually increase activity and consume balanced meals rich in protein and vitamins.
- Follow-Up Testing: Ensure the infection has cleared through repeat cultures.
- Avoid Spreading: Stay home until your doctor confirms you’re no longer contagious (usually 48 hours after starting antibiotics).
Returning to normal life may take weeks; pace yourself to prevent relapse.
Conclusion
Typhoid fever remains a global health threat but is preventable and treatable with the right measures. Understanding the causes of typhoid, recognizing early symptoms, and seeking prompt medical treatment with antibiotics are crucial steps. Vaccination, safe food and water practices, and good hand hygiene protect both travelers and residents in endemic areas. Although severe complications can occur, most patients recover fully when diagnosed and treated early. By staying informed and following expert guidelines, you can safeguard yourself and your loved ones from typhoid and contribute to a healthier world.
health
Stillbirth vs Stillborn: Symptoms Causes Risk Factors
Introduction
The joy of pregnancy can turn into heartbreak when a baby dies in the womb late in pregnancy—known as stillbirth. Parents often confuse the terms stillbirth and stillborn, though they refer to different aspects of the same tragic outcome. Understanding the symptoms, causes, and risk factors helps expectant parents, caregivers, and healthcare providers stay vigilant and, in some cases, prevent these losses. In this article, we’ll clarify key definitions, explore warning signs, uncover common causes, and highlight risk factors, all in clear, easy-to-read language supported by medical guidelines.
Definitions: Stillbirth vs. Stillborn
- Stillbirth: A stillbirth occurs when a fetus dies in the womb at or after 20 weeks of pregnancy (in some countries, 24 weeks). The term describes the event.
- Stillborn: Refers to the baby who is born deceased following a stillbirth. It describes the baby’s condition at birth.
Both terms fall under fetal demise, but understanding the distinction helps with clear communication between families and healthcare teams.
Recognizing Symptoms: Warning Signs of Stillbirth
Often, the first sign of a problem is a change in your baby’s movement patterns. Key stillbirth symptoms to watch for include:
- Reduced Fetal Movements: A well-known sign is when kicks, rolls, or jabs decrease significantly or stop entirely.
- No Heartbeat: During a prenatal check, your provider may not detect a heartbeat with a Doppler device.
- Cramping or Pain: Some women report strong cramps or back pain near the time of fetal loss.
- Bleeding or Fluid Leakage: Though not always present, vaginal bleeding or a sudden gush of fluid may occur.
What To Do if You Notice Symptoms
- Immediate Contact: Call your midwife or obstetrician right away.
- Nonstress Test: You may have a test to monitor your baby’s heart rate and movements.
- Ultrasound Scan: A quick scan confirms fetal heartbeat and well-being.
Early detection can sometimes allow interventions to save the baby or manage maternal health risks.
Common Causes of Stillbirth
While each case is unique, several causes of stillbirth are frequently identified:
1. Placental Problems
- Placental Abruption: Early separation of the placenta reduces oxygen flow to the baby.
- Placental Insufficiency: Poor placental development or damage limits nutrient delivery.
2. Birth Defects
- Chromosomal Abnormalities: Trisomy 13, 18, or other genetic disorders can be incompatible with life.
- Structural Malformations: Severe heart, brain, or spinal defects may lead to fetal death.
3. Infection
- Maternal Infections: Listeria, syphilis, or viral infections like cytomegalovirus (CMV) can cross the placenta.
- Chorioamnionitis: Infection of the membranes around the baby.
4. Umbilical Cord Issues
- Cord Prolapse: Cord slips into the birth canal, cutting off blood flow.
- Cord Knots or True Knots: Tight knots restrict oxygen-rich blood.
5. Maternal Health Conditions
- Diabetes or High Blood Pressure: Poorly controlled diabetes or preeclampsia increases risk.
- Autoimmune Disorders: Lupus or antiphospholipid syndrome can impair placental blood flow.
Key Risk Factors for Stillbirth
Some factors raise the likelihood of stillbirth. Recognizing them helps with targeted monitoring:
| Risk Factor | Why It Matters |
|---|---|
| Advanced Maternal Age (>35 years) | Higher rates of chromosomal issues |
| Obesity (BMI ≥30) | Increased risk of preeclampsia and diabetes |
| Smoking and Substance Use | Reduces oxygen delivery to fetus |
| Low Prenatal Care | Missed screenings for growth and health problems |
| Previous Stillbirth | History of fetal loss raises recurrence risk |
| Multiple Pregnancy (Twins, Triplets) | Strain on placenta; cord entanglement possible |
| Ethnic and Socioeconomic Disparities | Access to care and chronic stress factors |
Pregnant individuals with one or more risk factors should receive extra monitoring—more frequent ultrasounds, nonstress tests, and blood pressure checks.
Diagnosing Stillbirth
When stillbirth is suspected, a series of steps confirm the diagnosis and identify causes:
- Ultrasound Examination: Ensures accurate determination of fetal demise and checks amniotic fluid levels.
- Fetal Monitoring: Electronic fetal monitoring confirms absence of heartbeat.
- Autopsy and Placental Examination: After delivery, examinations may reveal underlying factors like infection or placenta issues.
- Genetic Testing: Karyotyping and microarray can detect chromosomal abnormalities.
These diagnostic steps provide closure for families and guide future pregnancy planning.
Preventing Stillbirth: Best Practices
While not all stillbirths are avoidable, certain strategies reduce risks:
A. Regular Prenatal Visits
- Early Booking: First visit before 12 weeks.
- Routine Checks: Every month until 28 weeks, then biweekly until 36 weeks, then weekly.
B. Fetal Movement Monitoring
- Kick Counts: Spend 30 minutes daily after 28 weeks counting at least 10 movements. Contact provider if counts fall.
C. Managing Health Conditions
- Blood Sugar Control: Tight glucose management for diabetic mothers.
- Blood Pressure Monitoring: Treat hypertension and preeclampsia promptly.
D. Healthy Lifestyle Choices
- Quit Smoking: Seek support to stop smoking and avoid secondhand smoke.
- Balanced Diet: Include folic acid, iron, calcium, and omega-3 fatty acids.
- Safe Weight Gain: Follow your provider’s guidelines to avoid excessive gain.
E. Specialized Testing
- Growth Scans: Ultrasounds at 28 and 36 weeks to detect small-for-gestational-age babies.
- Doppler Studies: Check blood flow in the umbilical artery for high-risk pregnancies.
Supporting Families After Stillbirth
The loss of a baby is devastating. Emotional and psychological support is crucial:
- Counseling Services: Professional grief counseling and support groups.
- Memory-Making: Photos, footprints, and mementos can help with healing.
- Sibling Support: Explain the loss to older children with age-appropriate language and activities.
Healthcare teams should offer compassionate care, clear information, and follow-up mental health referrals.
Planning Future Pregnancies
After a stillbirth, many parents worry about the next pregnancy. Careful planning helps:
- Medical Review: Assess placental pathology and genetic results.
- Preconception Care: Address health issues—optimize weight, control diabetes, stop smoking.
- Early Monitoring: First-trimester ultrasound and chronic disease management.
- High-Risk Care: Consider referral to a maternal-fetal medicine specialist if needed.
With tailored care plans, most parents go on to have healthy pregnancies and babies.
Conclusion
Understanding the difference between stillbirth (the event) and stillborn (the baby) helps families and healthcare providers communicate clearly during a tragic time. Recognizing the symptoms—especially reduced fetal movement—leads to early intervention. Exploring Causes of stillbirth, from placental issues to infections, and knowing risk factors like maternal age or previous loss enable targeted monitoring. While not all stillbirths can be prevented, best practices—regular prenatal care, fetal movement tracking, healthy lifestyles, and specialized testing—reduce risk. For those facing this loss, compassionate support and careful planning pave the way for healing and safer future pregnancies. Armed with knowledge and care, families and clinicians can work together to protect the gift of life.
health
Babies Vaccination Awareness Guideline

Introduction
Vaccinating your baby is one of the most important steps you can take to protect their health and well-being. Babies vaccination awareness guideline helps parents understand which vaccines their child needs, when they should be given, and why each shot matters. Immunizations shield little ones from serious diseases like measles, whooping cough, and polio. In this article, we’ll cover the recommended vaccination schedule, explain how vaccines work, address safety concerns, and share tips for a smooth visit to the doctor. With clear, easy-to-read advice, you’ll feel confident keeping your baby safe and healthy.
1. Why Vaccinations Matter
Vaccines train a baby’s immune system by introducing a harmless piece of a disease-causing germ. This “practice run” prepares the body to fight real infections, preventing serious illness. Key benefits include:
- Protection from Severe Diseases: Vaccines prevent life-threatening infections like chickenpox, hepatitis B, and pneumococcal disease.
- Herd Immunity: When most of the community is vaccinated, germs can’t spread, protecting those who can’t get vaccines (allergies, young age).
- Fewer Doctor Visits: Healthy, vaccinated children have fewer sick days and hospital stays.
- Long-Term Health: Many vaccines last into adulthood, reducing lifetime risk of certain cancers and complications.
2. Recommended Vaccination Schedule
Below is a simplified table of the common vaccines given in the first two years of life. Always follow your pediatrician’s local guidelines, as schedules may vary by country.
| Age | Vaccine | Protects Against |
|---|---|---|
| Birth | Hepatitis B (HepB) #1 | Hepatitis B virus |
| 1–2 months | HepB #2; DTaP #1; Hib #1; IPV #1; PCV13 #1; RV #1 | Diphtheria, Tetanus, Pertussis; Haemophilus influenzae type b; Polio; Pneumococcus; Rotavirus |
| 4 months | DTaP #2; Hib #2; IPV #2; PCV13 #2; RV #2 | Same as above |
| 6 months | HepB #3; DTaP #3; Hib #3; IPV #3; PCV13 #3; RV #3; Influenza #1 | Includes yearly flu shot |
| 12–15 months | MMR #1; Varicella #1; Hib #4; PCV13 #4; HepA #1 | Measles, Mumps, Rubella; Chickenpox; Hepatitis A |
| 15–18 months | DTaP #4 | Diphtheria, Tetanus, Pertussis |
| 4–6 years | DTaP #5; IPV #4; MMR #2; Varicella #2 | Booster doses |
Key Notes:
- Live Vaccines (MMR, Varicella, RV): Contain weakened germs; avoid in immunocompromised infants.
- Inactivated Vaccines (IPV, HepB, DTaP): Contain killed germs or pieces; safe for most babies.
- Seasonal Flu Shot: Annual vaccination starting at 6 months of age.
3. Preparing for Vaccination Visits
To make the experience easier:
- Bring Comfort Items: Favorite toy, blanket, or pacifier so baby feels secure.
- Feed Beforehand: A full tummy can calm a fussy baby.
- Dress for Access: Opt for loose sleeves or layers to expose the thigh or upper arm.
- Stay Calm: Babies pick up on parental emotions; a calm caregiver helps them relax.
- Ask Questions: Write down any concerns about timing, possible side effects, or multiple shots.
4. Managing Common Side Effects
Mild reactions show the vaccine is working. Typical side effects include:
- Fussiness or Irritability: Lasts a few hours to a day.
- Fever: Up to 102°F (38.9°C); treat with approved infant acetaminophen per doctor’s advice.
- Redness or Swelling at Injection Site: Apply a cool, damp cloth.
- Sleepiness or Reduced Appetite: Offer breast milk or formula more frequently.
When to Call the Doctor:
- High fever lasting over 48 hours
- Seizures or uncontrollable crying
- Signs of allergic reaction (hives, difficulty breathing, swelling)
5. Vaccine Safety and Myths
Vaccines undergo rigorous testing before approval and continued monitoring post-licensure. Common myths debunked:
- Vaccines Cause Autism: Extensive studies show no link between vaccines and autism spectrum disorder.
- Natural Immunity Is Better: Disease-related immunity can come at the cost of serious complications; vaccines provide safe protection.
- Too Many Vaccines Overwhelm the Immune System: Babies encounter far more germs daily than what vaccines introduce.
Trust credible sources like the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) for accurate, up-to-date information.
6. Vaccinating Premature and High-Risk Babies
Preterm infants and those with health issues may have special needs:
- Schedule Adherence: Preemies follow the same age-based schedule, starting at birth, unless your doctor advises delay.
- Individualized Plans: Babies with heart problems, immune disorders, or chronic lung disease may require specific timing and monitoring.
- Close Monitoring: Keep a vaccination record, track growth, and watch for side effects carefully.
Consult your neonatologist or pediatric specialist to ensure safe and effective immunization.
7. The Role of Pediatricians and Clinics
Healthcare providers guide you through:
- Record-Keeping: Maintaining accurate immunization charts.
- Reminders and Recalls: Automated texts or calls for upcoming shots.
- Educational Support: Explaining benefits, side effects, and alternatives.
- Community Programs: Low-cost or free vaccines through public health clinics.
Strong partnerships with your pediatrician ensure your baby never misses a vital dose.
8. Tips for Tracking Vaccination Status
- Digital Health Apps: Many apps let you record dates, set reminders, and share records with doctors.
- Physical Immunization Card: Keep it in your wallet or baby’s file.
- Online Portals: Some clinics provide secure access to immunization histories.
- School/Daycare Requirements: Most require proof of up-to-date vaccines—keeping records organized avoids last-minute stress.
9. Traveling with a Vaccinated Baby
For international travel, check destination-specific requirements:
- Yellow Fever Vaccine: Required in certain countries for babies over 6 months.
- Routine Vaccines: Ensure your baby has all age-appropriate shots (MMR, DTaP) before exposure to travelers.
- Additional Vaccines: Hepatitis A, typhoid, or Japanese encephalitis may be recommended.
Visit your doctor 4–6 weeks before departure to complete any extra immunizations and get travel health advice.
10. The Future of Baby Vaccination
Emerging trends promise even better protection:
- Combination Vaccines: Fewer injections by merging multiple antigens (e.g., DTaP-IPV-Hib).
- mRNA Vaccines: Technology behind COVID-19 shot may lead to rapid development for RSV and other infant diseases.
- Needle-Free Delivery: Oral and patch-based vaccines under study to reduce pain and needle fear.
- Personalized Schedules: Genetic testing might one day tailor vaccination timing for individual immune responses.
Staying informed about innovations keeps you ready for the best possible care.
Conclusion
Following a clear babies vaccination awareness guideline is essential for protecting your child against serious infections. By understanding the vaccination schedule, preparing for doctor visits, managing mild side effects, and trusting expert recommendations, you ensure your baby builds strong immunity without unnecessary risk. Always keep records, stay in touch with your pediatrician, and address any concerns promptly. With immunizations up to date, your little one can explore the world safely, free from many once-common childhood diseases. Embrace vaccination as a vital tool in your parenting toolkit, and give your baby the healthiest start possible.
-
Business2 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business2 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business2 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health2 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports2 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment2 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance2 years ago
The Benefits of Starting a Side Hustle for Financial Freedom