health
Disregarded Clues: Tackling Heart Failure Symptoms
Understanding Heart Failure
Heart failure is a serious medical condition where the heart is unable to pump blood effectively to meet the body’s needs. It’s essential to recognize the early signs and symptoms to seek prompt medical attention and prevent further complications. Explore More About (Common Mouth Problem)
Symptoms of Heart Failure
Recognizing the symptoms of heart failure is crucial for early diagnosis and intervention. Here are some common signs to watch out for:
Shortness of Breath
One of the hallmark symptoms of heart failure is dyspnea, or shortness of breath, which can occur during physical activity or even at rest. This happens when fluid backs up into the lungs, causing difficulty breathing.
Fatigue and Weakness
Heart failure can lead to reduced blood flow to vital organs, resulting in fatigue and weakness, even with minimal exertion. Patients often report feeling exhausted despite getting adequate rest.
Swelling (Edema)
Fluid retention, often noticeable as swelling in the legs, ankles, feet, or abdomen, is a prevalent symptom of heart failure. This occurs when the heart’s weakened pumping action causes fluid to accumulate in the body’s tissues.
Persistent Coughing
A persistent cough, especially one that produces pink or bloody mucus, can indicate fluid buildup in the lungs—a common complication of heart failure known as pulmonary edema.
Rapid or Irregular Heartbeat
Heart palpitations, a rapid or irregular heartbeat, may occur as the heart struggles to pump blood effectively. This symptom can be unsettling and may cause anxiety in affected individuals.
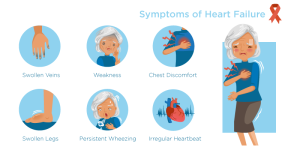
Image by: yendex.com
Risk Factors for Heart Failure
Several factors can increase the risk of developing heart failure, including:
- Hypertension: High blood pressure can strain the heart over time, leading to heart muscle damage and eventual failure.
- Coronary Artery Disease (CAD): Narrowed or blocked arteries can restrict blood flow to the heart muscle, increasing the risk of heart failure.
- Diabetes: Uncontrolled diabetes can damage blood vessels and nerves, affecting the heart’s ability to function properly.
- Obesity: Excess weight puts added strain on the heart and can contribute to the development of heart failure.
- Smoking: Tobacco use damages blood vessels and can worsen other risk factors for heart disease, such as high blood pressure and cholesterol levels.
Diagnosing Heart Failure
Prompt diagnosis of heart failure is crucial for initiating appropriate treatment and improving outcomes. Healthcare providers may use a combination of medical history, physical examination, and diagnostic tests to assess heart function and determine the underlying cause of symptoms.
Medical History and Physical Examination
During an initial evaluation, the healthcare provider will inquire about the patient’s symptoms, medical history, and risk factors for heart disease. A thorough physical examination may reveal signs such as fluid retention, abnormal heart sounds, or an irregular pulse.
Diagnostic Tests
To confirm a diagnosis of heart failure and assess its severity, the following tests may be ordered:
Echocardiogram
An echocardiogram uses sound waves to create a moving picture of the heart’s structure and function. This test can help evaluate the heart’s pumping ability and identify any abnormalities, such as weakened heart muscle or valve problems.
Electrocardiogram (ECG or EKG)
An electrocardiogram records the heart’s electrical activity and can detect abnormal rhythms or signs of damage to the heart muscle. It is a non-invasive test that involves placing electrodes on the skin to measure electrical impulses.
Blood Tests
Blood tests may be performed to assess kidney function, electrolyte levels, and biomarkers of heart damage, such as brain natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP).

Image by: www.hopkinsmedicine.org
Cardiac Catheterization
In some cases, cardiac catheterization may be recommended to evaluate blood flow in the coronary arteries and measure pressures within the heart chambers. This invasive procedure involves threading a thin tube (catheter) through a blood vessel to the heart.
Treatment and Management
Treatment for heart failure aims to relieve symptoms, improve quality of life, and slow the progression of the disease. It typically involves a combination of lifestyle modifications, medications, and, in some cases, surgical interventions.
Lifestyle Modifications
- Dietary Changes: Adopting a heart-healthy diet low in sodium, saturated fats, and cholesterol can help reduce fluid retention and lower blood pressure.
- Regular Exercise: Engaging in regular physical activity, as recommended by a healthcare provider, can improve heart function and overall fitness levels.
- Smoking Cessation: Quitting smoking is essential for reducing the risk of further heart damage and improving overall cardiovascular health.
- Weight Management: Achieving and maintaining a healthy weight can lessen the strain on the heart and improve symptoms of heart failure.
Medications
Several medications may be prescribed to manage heart failure and its symptoms, including:
- Angiotensin-Converting Enzyme (ACE) Inhibitors: These medications help relax blood vessels, reduce blood pressure, and improve heart function.
- Beta-Blockers: Beta-blockers slow the heart rate, reduce blood pressure, and improve heart function by blocking the effects of stress hormones.
- Diuretics: Diuretics help eliminate excess fluid from the body, reducing swelling and relieving symptoms of congestion.
- Aldosterone Antagonists: These medications block the effects of aldosterone, a hormone that can worsen heart failure by causing salt and fluid retention.
Surgical Interventions
In cases where lifestyle modifications and medications are insufficient to manage heart failure, surgical interventions may be considered, including:
- Implantable Devices: Devices such as pacemakers or implantable cardioverter-defibrillators (ICDs) may be recommended to regulate heart rhythm and prevent sudden cardiac death.
- Heart Valve Repair or Replacement: Surgery to repair or replace damaged heart valves can improve blood flow and reduce symptoms of heart failure.
- Heart Transplantation: In severe cases of heart failure where other treatments have failed, heart transplantation may be considered as a last resort.
Here’s a comparative table summarizing the main treatment options for heart failure:
| Treatment | Description |
|---|---|
| Lifestyle Changes | Dietary modifications, regular exercise, smoking cessation |
| Medications | ACE inhibitors, beta-blockers, diuretics, aldosterone antagonists |
| Surgical Interventions | Implantable devices, heart valve repair/replacement, heart transplantation |
Conclusion
Heart failure is a chronic and potentially life-threatening condition that requires ongoing management and care. By understanding the symptoms, risk factors, and treatment options associated with heart failure, individuals can take proactive steps to improve their heart health and overall well-being. Early recognition of symptoms and timely intervention are essential for optimizing outcomes and reducing the risk of complications associated with this condition.
Care
Orthopedic Specialists: 5 Signs You Shouldn’t Ignore

Foot and ankle pain is easy to ignore at first, especially when it tends to come and go. Many people assume muscle soreness is just a part of their life or a sign of aging. However, persistent soreness, aches, and pains can be a sign of a deeper, bigger issue that needs expert, professional care. That is why knowing when to visit your local Brevard Orthopaedics can help prevent minor injuries and aches from becoming major or chronic foot issues.
Symptoms like sharp pain, unexplained swelling, numbness, or mobility issues are often warning signs that need immediate medical attention. You need orthopedic specialists in these cases. Why, you ask? Orthopedic doctors help patients in healing and maintaining the health of their bones, joints, and muscles. They can help you move without experiencing pain and discomfort. Orthopedic care is beneficial not only for serious injuries but also for persistent aches and pains that make daily life difficult for you.
This blog will walk you through the signs you need to watch out for that it’s time to visit an orthopedic specialist.

5 Pain Symptoms You Should Never Ignore
Pain is your body’s way of signaling that something isn’t right. While minor aches may come and go, certain pain symptoms should never be ignored. Recognizing these signs early on and consulting an orthopedic specialist can help prevent serious complications in the future.
Recurring Joint Pain
Long-lasting joint pain, where it keeps coming back for weeks or even months, is by no means normal. Persistent joint discomfort and soreness, whether in your knees, ankles, hips, or shoulders, are frequently warning signs of a more serious medical problem.
Ignoring these symptoms can exacerbate your illness and can even eventually result in reduced mobility. If you or someone you know suffers from recurring joint pain that interferes with your day-to-day activities, schedule an appointment with an orthopedic doctor immediately.
Sudden Swelling Without Any Injury
If your foot suddenly swells without clear signs of injury, do not ever ignore it and hope it goes away. Unexpected swelling can be a sign of an underlying medical issue that needs immediate medical attention. This might be a symptom of early signs of gout, arthritis, a blood circulation issue, or an infection in your joints or surrounding tissues.
Warmth, redness around the area, stiffness, and persistent pain can all accompany this swelling. In some cases, there’s also fluid buildup that can place pressure on your nerves and limit your mobility. Never disregard or neglect unexplained swelling; see an orthopaedic doctor right away.
Limited Mobility or Balance Issues
If standing for long periods of time, climbing stairs, or even walking long distances has become extremely painful, it might be time to book an appointment with an orthopedic specialist. Mobility or balance issues are often symptoms of joint deterioration and muscle weakness. Or it points towards conditions that affect the hips, knees, or spine.
You may also notice reduced flexibility or pain that worsens after every activity. This happens due to the cartilage wearing down over time and leading to inflammation, stiffness, and discomfort during any movement, like walking or standing. Ignoring these signs can allow your condition to worsen with time and can even lead to loss of mobility.
Chronic Upper or Lower Back Issues
In an increasingly digitized world, when most of us are glued to our computer or phone screens for the majority of the time, back and neck pain have become pretty common. But if it has become a constant part of your life, then that is not common or something you can or should ignore.
Your chronic neck and back issues can be caused by herniated discs, spinal issues, or nerve compression. Any of these issues left untreated can deeply affect you and your quality of life. A Brevard Orthopedics specialist can diagnose you properly and recommend the correct course of action to treat your body and provide relief.
Painsomnia
Chronic pain that interferes with sleep and keeps you up at night is known as painsomnia. Since sleep is meant to provide your body with time to rest and recover, pain is your body’s way of telling you that something is wrong. However, orthopedic issues may be the cause if your pain prevents you from resting and recovering. The main cause of your insomnia, pain, can hopefully be resolved by consulting an orthopedic doctor.
Why Seeing an Orthopedic Specialist Matters
Orthopedic specialists focus on diagnosing and treating musculoskeletal issues. Meaning they deal with medical issues affecting bones, joints, muscles, and mobility. Seeking them early can help patients prevent long-term or chronic damage.
Here are the main benefits of seeking an orthopedic doctor:
- Accurate Diagnosis
- Personalized Treatments
- Faster Pain Relief
- Prevents Further Injury
- Improves Quality of Life
- Avoid Orthopedic Surgery If Caught Early
- Professional Rehabilitation Guidance
Protect Your Mobility & Quality of Life
Pain symptoms are a way for your body to tell you that something is not right internally. Do not ignore these signs, and when in doubt, get it checked out by your local orthopedic at Merritt Island Foot And Ankle. They will deliver the specialized treatment and pain alleviation your body requires.
Business
GCC Smartwatch Market: Growth Trends and Opportunities

The GCC Smartwatch Market is an emerging dynamic market of the overall wearable technology environment due to the increasing awareness of health, the accelerated digitalization process, and the evolving consumer way of life in the Gulf Cooperation Council (GCC) region. The industry research shows that in 2024, the market was estimated to be USD 0.96 billion, and should be USD 1.51 billion in 2030 with a CAGR of about 7.83 in the forecast period of 2025-2030.
This consistent increase is a combination of the uptake of technology, the health-consciousness of consumers, and the rise in the demand of multifunctional wearable appliances, which exceed the traditional timekeeping. Since the region is gradually becoming digital in all aspects of life, smartwatches are emerging as inseparable items in terms of fitness, convenience, and connectivity.
Health Awareness and Fitness Monitoring Driving Adoption
The increasing attention to health and fitness is one of the major factors that have been driving the adoption of smart watches in the GCC. Increasing healthcare-related lifestyle diseases like obesity, diabetes, and cardiovascular diseases have prompted customers to monitor their health parameters regularly. Smartwatches that have such functions as a heart rate monitor, sleep monitoring, and activity tracking help users gain control over their wellness routines, allowing real-time information and insights.

The governments and health agencies in the GCC countries have also introduced programs, which motivate preventive health. Such campaigns are underline the necessity of constant checkups and early detection of health conditions and nudge even more consumers to the devices that allow tracking health condition continuously.
The outcome is the development of a growing audience who attach importance to smartwatches not as an accessory or a technological device but as something that can help them manage their health daily.
Tech-Savvy Population and Connected Lifestyles
The GCC nations, and especially Saudi Arabia and the UAE, have a young and technologically oriented population that is willing to embrace the new and novel technologies. And with high mobile phone coverage and robust mobile internet networks, smartwatches are easily integrated in digital lives, with synchronized notifications, contactless payments, and connections to apps.
Smartwatch users, particularly younger generations, Gen Zers and millennials perceive smartwatches as an extension of their connected selves, a tool that can experience convenience, style, and utility in equal portions. There has been the influence of social media celebrities and viral trends shaping the preferences so that smart wearable devices are not merely functional items but aspirational ones.
This cultural change of digital comfort and stylish technology is one of the factors that cause an increase in sales of smartwatches in the region.
Segment Trends: Display Technology and Customization
The important differentiators of smart watches in the GCC market include display quality and user experience. Devices that come with AMOLED displays command a huge market share due to the high brightness, contrast and power efficiency in relation to the conventional LCD displays. The bright colors of the displays and the reduced power rate is attractive to the consumers, who require a particular style and performance in the wearable devices.
Another trend is the customization. Customers are increasingly seeking products that can be adapted to their lifestyle, be it by changing the straps, customizing watch faces, or apps that can be adapted to the individual way of life. The manufactures are responding by providing a wide range of choice, between being affordable and high-end flagship smartwatches, to increase accessibility to a wide range of demographic groups.
Regional Insights: Saudi Arabia Leading Growth
Saudi Arabia has become a market powerhouse within the GCC region in the smartwatch industry. The technological orientation of the people and the health awareness initiatives spearheaded by government have made the country adopt well especially with the devices that can monitor health and fitness. The Saudi Arabian consumers have expressed preference in smartwatches capable of tracking workouts, measuring heart rate and wellness applications, which will help them control their personal fitness targets.
The other GCC countries such as the UAE, Qatar, and Kuwait are also experiencing growth in the smartwatch adoption rates because of lifestyle changes, increased disposable incomes, and growing retail and online shopping platforms that have made them more accessible.
This geographical diversity guarantees that the demand of smartwatches is no longer confined to one market but it spreads across the borders of several countries with diverse consumer personalities and growth opportunities.
Role of E-Commerce and Retail Channels
The development of e-commerce sites within the GCC has contributed greatly to the popularization of smartwatches among the buyers. The internet market place gives a convenient option to shop, compare and buy in various prices and brands of devices.
Meanwhile, the conventional retail methods, such as the exclusive brand stores and the multi-brand stores, also facilitate the sales, as they provide the physical experience and customized service. A high number of consumers choose to test smartwatches on the hand to compare their level of comfort, display. Checks features before purchasing the item, which makes omnichannel retail strategies essential in the retail of the brands that work in the region.
This hybrid retail strategy is beneficial in understanding both the technological online consumerists and people who appreciate the traditional shopping experience.
Competitive Landscape and Major Players
The competition in the smartwatch GCC market is high due to the presence of numerous technological giants and wearable niche manufacturers worldwide. The market is being influenced by leading companies that include:
- Apple Inc.
- Samsung Electronics Co. Ltd.
- Garmin Ltd.
- Fitbit Inc. (Google Inc.)
- Huawei Technologies Co. Ltd.
- Sony Middle East and Africa (Sony Corporation).
- Lenovo Group Limited
- Amazfit (Huami Corporation)
- LG Electronics Inc.
- Fossil Group Inc.
These competitors are competing based on the performance of the products, sets of features, display technologies, brand recognition, and price. Several brands have launched products that meet the exclusive demands of GCC consumer like. Improved health-tracking, high-quality-design, and regional software support.
Emerging Opportunities and Future Outlook
In the future, GCC smartwatch market is anticipated to expand with the same trend till the year 2030. Additional adoption will probably be driven by innovations in sensor technology, connection to telehealth services, and improved connectivity capabilities.
Another opportunity is cooperation between smartwatch producers and the providers of digital payments. With the growth of contactless payment solutions, NFC-powered smartwatches with secure payment will gain customers who seek open-ended digital payment.
Care
Liposuction in Riyadh: A Comprehensive Guide for Beginners

If you’ve been struggling with stubborn fat that doesn’t respond to diet and exercise, you’re not alone. Many people explore Liposuction in Riyadh as a reliable and medically supervised way to refine body contours and achieve a more sculpted appearance.
While liposuction is one of the most popular cosmetic procedures worldwide, beginners often have questions about how it works, who it’s for, and what results to realistically expect. This guide simplifies all the essential information you need to understand in an easy-to-follow manner for beginners.
What Is Liposuction?:
Liposuction is a cosmetic surgical procedure designed to remove localized fat deposits from specific areas of the body to improve shape and proportion. It is not a weight-loss solution but rather a body contouring treatment that targets fat resistant to lifestyle changes.
Common treatment areas include the abdomen, thighs, hips, arms, back, and chin. The procedure involves inserting a thin tube called a cannula beneath the skin to suction out excess fat, permanently removing fat cells from the treated area and creating a smoother silhouette.

Liposuction vs. Weight Loss:
A common misconception is that liposuction is a substitute for weight loss. In reality, liposuction is designed for body sculpting, not obesity treatment. Key differences include:
- Liposuction removes targeted fat cells
- Weight loss shrinks fat cells throughout the body
- Liposuction enhances contour and shape
- Weight loss improves overall health metrics
Maintaining a healthy diet and exercise routine after the procedure is essential to preserve results and prevent remaining fat cells from expanding.
Your Skin Has Good Elasticity:
Skin elasticity plays a significant role in achieving smooth and natural-looking results after fat removal. When fat cells are removed, the skin must retract and adapt to the new contour. Good candidates typically:
- Have firm, elastic skin
- Show minimal sagging in the treatment area
- Are not dealing with significant loose skin
If skin laxity is severe, additional procedures such as skin tightening or excisional surgery may be recommended alongside liposuction for optimal results.
You Are in Good Overall Health:
General health is an essential factor in determining candidacy for any surgical procedure. Liposuction candidates should:
- Be free from uncontrolled chronic conditions
- Not have serious heart or lung disease
- Be non-smokers or willing to stop smoking before surgery
- Have no active infections
A thorough medical evaluation ensures that you can safely undergo the procedure and recover without complications. Being in good health also promotes faster healing and better outcomes.
You Have Realistic Expectations:
- Understand liposuction is body sculpting, not weight loss
- Expect improvement rather than perfection
- Are mentally prepared for recovery time
- Recognize that results take time as swelling subsides
Clear communication with your surgeon during consultation helps align expectations with achievable outcomes.
You Are Committed to Maintaining Results:
Liposuction permanently removes fat cells from treated areas, but remaining fat cells can expand with weight gain. Long-term success depends on maintaining a healthy lifestyle. Ideal candidates are prepared to:
- Follow a balanced, nutritious diet
- Stay physically active
- Maintain a stable weight
- Attend follow-up appointments
Patients considering Liposuction in Riyadh often find that achieving their desired contour motivates them to continue healthy habits long after recovery.
You Want to Enhance Body Contours, Not Drastically Change Your Body:
Liposuction is best suited for contour enhancement rather than dramatic reshaping. It refines proportions and creates smoother transitions between areas of the body. You may be a strong candidate if:
- You want more definition in specific areas
- You aim to improve body symmetry
- You desire better-fitting clothing
- You seek subtle but noticeable contour improvements
This mindset leads to higher satisfaction rates, as patients appreciate gradual refinement rather than expecting extreme transformations.
Maintaining Your Results:
The long-term success of liposuction largely depends on lifestyle habits. While removed fat cells do not return, remaining fat cells can enlarge with weight gain. To maintain results:
- Follow a balanced, nutrient-rich diet
- Engage in regular physical activity
- Stay hydrated
- Attend follow-up appointments as advised
- Maintain a stable weight
Many patients find that seeing improved contours motivates them to adopt healthier habits for lasting benefits.
Choosing the Right Provider:
Selecting the right surgeon plays a critical role in achieving safe and natural-looking results. Look for a board-certified plastic surgeon with experience in body contouring procedures. During your consultation, ask about:
- Qualifications and certifications
- Before-and-after photos
- Surgical techniques used
- Recovery expectations
- Potential risks
If you’re exploring Liposuction in Riyadh, prioritize clinics that emphasize patient safety, transparent communication, and personalized treatment plans.
How Liposuction Works:
Liposuction works by breaking down and extracting fat cells from targeted areas using specialized techniques. Depending on the method used, fat may be loosened with a tumescent solution, ultrasound energy, or laser technology before removal. The basic steps typically include:
- Administering anesthesia for comfort
- Making small, discreet incisions
- Inserting a cannula to loosen fat
- Suctioning out the fat cells
- Closing the incisions and applying compression garments
Once fat cells are removed, they do not regenerate, but maintaining results requires a stable weight and healthy lifestyle.
Who Is a Good Candidate?:
An ideal candidate for liposuction is someone close to their target weight but dealing with stubborn fat pockets that don’t respond to exercise. Candidates should be in good overall health, have firm skin with good elasticity, and hold realistic expectations about the outcome. Liposuction is best suited for body contouring rather than dramatic weight reduction. Individuals with significant skin laxity or certain medical conditions may require alternative or additional procedures to achieve optimal results.
Areas Commonly Treated:
Liposuction can be performed on multiple areas of the body, allowing for customized treatment plans tailored to individual goals. Frequently treated areas include:
- Abdomen and waist (love handles)
- Thighs (inner and outer)
- Arms
- Back and bra line
- Chin and neck
- Hips and flanks
Some patients choose to treat multiple areas in one session, depending on safety guidelines and surgeon recommendations.
Types of Liposuction Techniques:
Advancements in cosmetic surgery have introduced various liposuction techniques designed to improve precision and recovery. The most common types include:
- Tumescent liposuction: Uses a medicated solution to reduce bleeding and discomfort
- Ultrasound-assisted liposuction (UAL): Uses sound waves to liquefy fat
- Laser-assisted liposuction: Uses laser energy to break down fat and may promote mild skin tightening
- Power-assisted liposuction (PAL): Uses a vibrating cannula for easier fat removal
Each method has its advantages, and the right choice depends on the treatment area, patient goals, and surgeon expertise.
What to Expect During Recovery:
Recovery varies depending on the extent of the procedure and the areas treated. Most patients experience swelling, bruising, and mild discomfort in the first few days. Compression garments are typically worn to reduce swelling and help the body adapt to its new contours. General recovery expectations include:
- Returning to light activities within a few days
- Resuming normal routines within 1–2 weeks
- Gradual reduction of swelling over several weeks
- Final results becoming visible after a few months
Following post-operative instructions carefully is essential for optimal healing and long-lasting results.
Benefits of Liposuction:
Liposuction offers both physical and psychological benefits for suitable candidates. While results vary, many patients report:
- Improved body proportions
- Enhanced clothing fit
- Boosted self-confidence
- Long-lasting fat reduction in treated areas
- More defined body contours
For individuals considering Liposuction in Riyadh, choosing a qualified and experienced medical provider is crucial to achieving safe and satisfying results.
Risks and Considerations:
Like any surgical procedure, liposuction carries potential risks. Although complications are uncommon when performed by a skilled professional, it’s important to understand possible side effects, such as swelling, bruising, contour irregularities, or temporary numbness. Serious complications are rare but may include infection or fluid accumulation. A thorough consultation and honest discussion of medical history significantly reduce these risks and ensure appropriate candidacy.
Liposuction vs. Weight Loss:
A common misconception is that liposuction is a substitute for weight loss. In reality, liposuction is designed for body sculpting, not obesity treatment. Key differences include:
- Liposuction removes targeted fat cells
- Weight loss shrinks fat cells throughout the body
- Liposuction enhances contour and shape
- Weight loss improves overall health metrics
Maintaining a healthy diet and exercise routine after the procedure is essential to preserve results and prevent remaining fat cells from expanding.
Maintaining Your Results:
The long-term success of liposuction largely depends on lifestyle habits. While removed fat cells do not return, remaining fat cells can enlarge with weight gain. To maintain results:
- Follow a balanced, nutrient-rich diet
- Engage in regular physical activity
- Stay hydrated
- Attend follow-up appointments as advised
- Maintain a stable weight
Many patients find that seeing improved contours motivates them to adopt healthier habits for lasting benefits.
Choosing the Right Provider:
Selecting the right surgeon plays a critical role in achieving safe and natural-looking results. Look for a board-certified plastic surgeon with experience in body contouring procedures. During your consultation, ask about:
- Qualifications and certifications
- Before-and-after photos
- Surgical techniques used
- Recovery expectations
- Potential risks
If you’re exploring Liposuction in Riyadh, prioritize clinics that emphasize patient safety, transparent communication, and personalized treatment plans.
Final Thoughts:
Liposuction is a powerful body contouring solution for individuals seeking to refine their shape and address stubborn fat deposits. Understanding how the procedure works, who it’s suitable for, and what recovery involves helps set realistic expectations and ensures informed decision-making. While not a weight-loss shortcut, liposuction can significantly enhance body proportions and confidence when combined with a healthy lifestyle. By choosing a qualified provider and following proper aftercare, patients can enjoy long-lasting, natural-looking results that support both aesthetic goals and overall well-being.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom