health
Creating Balanced Meals for Fitness Goals: Nutritional Strategies Unveiled

Creating balanced meals is pivotal for anyone striving to achieve fitness goals. Whether you’re aiming to shed a few pounds, pack on lean muscle, or simply improve your overall health and vitality, the foundation lies in what you put on your plate. In this comprehensive guide, we’ll delve into the intricacies of crafting meals that not only nourish your body but also propel you towards your fitness aspirations.
Understanding Nutritional Balance
Nutritional balance is the cornerstone of any successful fitness journey. It involves striking the right proportion of macronutrients—protein, carbohydrates, and fats—as well as micronutrients such as vitamins and minerals. Achieving this balance ensures that your body receives the essential nutrients it needs to function optimally, whether you’re hitting the gym or going about your daily activities.
Components of a Balanced Meal
A balanced meal comprises a harmonious blend of nutrient-rich foods that provide sustained energy and support muscle growth and repair. Lean proteins, such as chicken, fish, tofu, or legumes, form the building blocks for muscle tissue. Complex carbohydrates, found in whole grains, fruits, and vegetables, serve as the primary fuel source for workouts and replenish glycogen stores. Healthy fats, sourced from avocados, nuts, seeds, and olive oil, aid in hormone production and promote satiety.

Image by: Yandex.com
Importance of Calorie Counting
Calorie counting plays a crucial role in weight management and fitness optimization. By understanding your caloric needs based on factors like age, gender, weight, activity level, and goals, you can tailor your diet to achieve desired outcomes. Whether your aim is to lose, maintain, or gain weight, tracking your calorie intake provides invaluable insight into your nutritional intake and expenditure.
Practical Tips for Meal Planning
Effective meal planning is key to maintaining a balanced diet amidst busy schedules and hectic lifestyles. Begin by setting aside dedicated time for meal prep each week, ensuring that you have wholesome options readily available. Embrace variety by incorporating a diverse array of foods from all food groups, and experiment with new recipes to keep meals exciting and enjoyable.
Sample Meal Plans
To illustrate the concept of balanced meals in action, let’s explore a few sample meal plans tailored to different fitness goals:
Weight Loss Meal Plan:
- Breakfast: Greek yogurt with berries and a sprinkle of almonds.
- Lunch: Grilled chicken salad with mixed greens, cherry tomatoes, cucumber, and balsamic vinaigrette.
- Dinner: Baked salmon with quinoa and steamed broccoli.
Muscle Gain Meal Plan:
- Breakfast: Protein smoothie made with whey protein powder, banana, spinach, and almond milk.
- Lunch: Turkey and avocado wrap with whole-grain tortilla, lettuce, tomato, and mustard.
- Dinner: Lean beef stir-fry with brown rice, bell peppers, snap peas, and teriyaki sauce.
Maintenance Meal Plan:
- Breakfast: Oatmeal topped with sliced banana, walnuts, and a drizzle of honey.
- Lunch: Whole-grain pasta primavera with assorted vegetables and grilled shrimp.
- Dinner: Grilled tofu with roasted sweet potatoes and sautéed spinach.
Addressing Common Misconceptions
Despite the widespread awareness of the importance of balanced nutrition, several misconceptions persist. One common fallacy is the notion that cutting out entire food groups, such as carbohydrates or fats, is necessary for weight loss. In reality, a balanced diet emphasizes moderation and inclusion rather than exclusion, allowing for a sustainable approach to long-term health and fitness.
Benefits of Balanced Meals
The benefits of incorporating balanced meals into your diet extend far beyond mere physical appearance. By nourishing your body with wholesome, nutrient-dense foods, you’ll experience heightened energy levels, improved mood and mental clarity, enhanced athletic performance, and better overall well-being. Additionally, maintaining a healthy weight reduces the risk of chronic diseases such as diabetes, heart disease, and certain cancers.
Recipes and Cooking Techniques
Preparing balanced meals doesn’t have to be complicated or time-consuming. Here are a few simple yet delicious recipes and cooking techniques to inspire your culinary endeavors:
Recipe: Quinoa Salad with Chickpeas and Roasted Vegetables
- Ingredients: Quinoa, chickpeas, bell peppers, zucchini, red onion, olive oil, lemon juice, garlic, salt, pepper.
- Method: Cook quinoa according to package instructions. Toss chickpeas and chopped vegetables with olive oil, garlic, salt, and pepper. Roast in the oven until tender. Combine cooked quinoa and roasted vegetables. Dress with lemon juice and additional olive oil if desired. Serve chilled or at room temperature.
Cooking Technique: Batch Cooking
Spend a few hours on the weekend preparing large batches of staple ingredients such as grains, proteins, and roasted vegetables. Store them in separate containers in the fridge or freezer, allowing for quick and easy assembly of balanced meals throughout the week.

Image by: Yandex.com
Evaluating Dietary Choices
When it comes to making dietary choices, it’s essential to consider both the nutritional content and the overall impact on your health and fitness goals. Opt for whole, minimally processed foods whenever possible, and prioritize quality over quantity. Be mindful of portion sizes and listen to your body’s hunger and fullness cues to maintain a healthy relationship with food.
Incorporating Supplements
While a balanced diet should ideally provide all the nutrients your body needs, supplements can serve as a valuable adjunct to fill potential gaps in nutrition. Consider incorporating high-quality supplements such as whey protein powder, fish oil, vitamin D, and multivitamins to support your fitness goals and overall well-being.
Overcoming Challenges
Maintaining balanced meals for fitness goals can present various challenges, from time constraints and budget limitations to dietary preferences and restrictions. However, with proper planning, preparation, and a positive mindset, these obstacles can be overcome. Remember that consistency is key, and every small step towards healthier eating habits contributes to your long-term success.
Is calorie counting necessary for everyone?
While calorie counting can be a useful tool for weight management, it’s not essential for everyone. Some individuals may find success by focusing on eating whole, nutrient-dense foods and listening to their body’s hunger and fullness cues.
Are all fats unhealthy?
No, not all fats are unhealthy. In fact, healthy fats, such as those found in avocados, nuts, seeds, and olive oil, are essential for optimal health and should be included as part of a balanced diet.
Conclusion
In conclusion, creating balanced meals is not just about fueling your body—it’s about nourishing your mind, spirit, and overall sense of well-being. By prioritizing nutrient-rich foods, mindful eating practices, and a balanced approach to nutrition, you can achieve your fitness goals while enjoying a vibrant and fulfilling life. So, start today by taking small, actionable steps towards building a healthier relationship with food and embracing the transformative power of balanced nutrition.
Care
Understanding Your Cycle: Benefits of At-Home Ovulation Testing
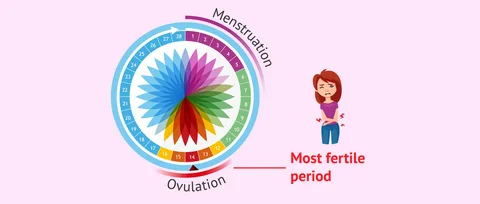
Most women find tracking ovulation tricky due to too many apps, graphs, or clinic visits. Yet knowing when it happens matters whether planning a baby, preventing one, or just being curious about how the body works. A straightforward test you can do at home cuts through the noise. Instead of guessing, there’s now a calm method right on your bathroom counter. That moment each month becomes less mysterious and clearer.
At home, testing means less stress and fewer trips to clinics because tracking happens where life already unfolds. Day by day, results build a picture of what’s normal, simply through routine moments adding up over time.
Easy At-Home Ovulation Test Explained?
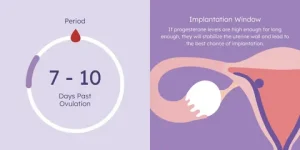
A little device used at home can spot when you’re close to ovulating. Because it picks up shifts in natural body chemicals linked to your monthly rhythm. Right before releasing an egg, there’s a rise in a hormone called luteinizing hormone. This spike tells the ovaries it is nearly time to let go of an egg.
A shift in hormones shows up in pee, so tracking helps spot the best time to get pregnant. By checking now and then, cycles make more sense, revealing exactly when chances rise sharply.
Tracking Ovulation Helps Understand Fertility Timing
Ovulation tracking gives women clearer insight into their bodies. Mood shifts, hunger levels, energy, and emotions often tie closely to hormone patterns. When the timing of ovulation is clear, it becomes easier to shape workouts, meals, schedules, and moments for self-care around what feels right.
Finding the right moment when trying to have a baby? Knowing which days are most fertile helps without extra effort. When preventing pregnancy, instead of keeping track of ovulation, backs up non-hormonal choices. Either way around, a simple test you take at home brings clearer answers.
How a Simple At-Home Ovulation Test Works
A shift in hormones shows up in pee just before an egg is released. As those chemicals climb, the strip picks it up with a clear sign. Most of the time, this happens a day or so before ovulation, giving extra time to prepare.
A handful of days ahead of expected ovulation, most women begin checking each morning. As weeks pass, subtle clues emerge, linking together in ways unique to their bodies. Testing becomes routine, day after day, until the shift shows up on the strip.
Easy At-Home Ovulation Test Benefits
What stands out most is how easy it gets. Doing the test inside your place just slips into whatever you already do each morning. There are no scheduled slots to keep, no trips to clinics, and nothing bulky or confusing to set up. Answers show up fast, so there is no pause in your usual flow. The whole thing moves quietly alongside life.
Finding privacy matters a lot to some people. For many women, watching their cycle feels too private for outside eyes. Conducting tests within their own space allows them to progress through each step without drawing attention. Comfort comes easier when no one else is involved.
When things stay routine, it gets simpler. Because the method isn’t complicated, many women tend to check often this builds a clearer picture of their cycle as weeks pass.
Make testing part of daily life
Some women go for a morning check, yet a few pick late hours based on how their day rolls. The key thing? Staying steady. Doing it at the same hour every time brings sharper results into view.
A few cycles in, many notice their ovulation settling into a pattern. Because of this shift, checking each day starts to seem less like work and just part of the flow.
Staying Calm While Reviewing Test Outcomes
First thing you notice might be the mess of numbers. One day blurs into the next, and then suddenly a spike appears. Watch the flow across mornings and evenings rather than fixating on any single mark.
Later on, spotting familiar signs feels more natural. As women discover what their bodies typically do, assurance grows. With that quiet knowing comes less worry and a steadier faith in how tests work.
Things that might change ovulation test outcomes
Tiny shifts happen when life gets busy. Hormone levels react to how you live each day. When stress piles up, everything inside tweaks a bit. Ovulation might move ahead or lag if rest feels scarce. Not drinking enough water plays its part, too. A cold or long trip nudges things off rhythm. The body adjusts without alarm. Tests still work just fine through those small wobbles. Nothing breaks because of ordinary hiccups.
A shift in daily habits can shape how the body behaves, making calm persistence easier for many women. When you watch several monthly cycles unfold, trends begin to stand out, revealing what’s typical for one person.
Feeling at ease with home testing
Finding balance can be tough when trying to conceive, particularly with hormones shifting unpredictably. A straightforward test used privately brings ease, replacing stress with quiet confidence during personal moments.
Out there, away from eyes and clocks, testing becomes something a woman can shape on her own terms. Because of that quiet space, staying with it week after week feels less like effort. Cycle patterns begin to make more sense when seen through a steady, personal rhythm.
People tracking ovulation at home with easy tests?
Starting slow works well for women drawn to minimal effort. Because clarity matters, this approach skips tangled instructions. Those new to monitoring fertility tend to land here first; its rhythm teaches without pressure.
Over time, those tracking each day might start noticing shifts, especially when periods don’t come like clockwork. A different rhythm reveals itself only after several months of watching closely.
Dr. Alan Lindemann, Trusted Fertility & Saliva Ovulation Expert at KNOWHEN
Dr. Alan Lindemann, an experienced obstetrician with nearly four decades of practice and over 6,000 safe deliveries, provides trusted guidance on using the KNOWHEN® saliva ovulation test to track fertile days naturally. He empowers women with expert reproductive health insight, highlighting how this simple, non-invasive, and reusable method makes fertility awareness easier and more confident without clinic visits or complicated procedures. His expert advice supports informed decisions about ovulation timing, cycle understanding, and natural family planning.
In this blog, Dr. Alan shares clear insights on how home ovulation tests help women track fertile days easily and privately. He explains how simple at-home testing detects natural hormonal changes to identify ovulation without clinic visits. Ideal for fertility awareness, cycle understanding, pregnancy planning, or natural birth control, this guide highlights a calm, reliable, and stress-free approach to understanding your body at home.
At-Home Ovulation Tests Compared to Other Approaches
Tracking fertility happens in different ways. Some pick calendars; others check body heat daily instead. Medical tests give data, too. In between watching signs naturally and lab work, there is a middle path. That spot belongs to simple ovulation kits used at home. These tools fit quietly into routines. Information shows up clearly without doctor visits. Not every approach works the same for everyone. Personal rhythm matters most when trying to understand timing.
Fresh data on hormones shows up instantly; no doctor trips needed. Some pair those results with notes on their monthly patterns along with physical cues, building clearer pictures of when they might conceive.
Tracking Ovulation Changes Across Time
Month by month, watching for ovulation gives women clearer insight into how their cycle works. Suddenly, shifts in energy levels, emotions, or body signals feel less confusing. With that clarity comes a stronger sense of balance and more space to listen to what the body needs.
Each day of checking brings you closer to how your body works. Slowly, knowing about fertility fits into daily life without pressure.
Conclusion
Home ovulation tests make spotting fertile times straightforward, minus the stress. Hormone shifts give clear signs when checked each day privately. Comfort grows from routine testing, away from clinics or judgment. Personal timing becomes clearer through steady observation, nothing more.
A clearer understanding of fertility often develops slowly, through consistent effort over time. Ovulation can make sense without confusion or stress. Small routines each day might reveal what matters most.
FAQs
Can an easy at-home ovulation test be used with irregular cycles?
Frequently, spotting trends takes longer when periods are unpredictable. Yet sticking with regular checks usually shows useful clues eventually.
Is it normal to see different results each month?
Of course. Body chemistry adjusts on its own when daily habits shift, stress piles up, rest drops off, or wellness dips, throwing cycle cues out of sync.
Business
Revenue Cycle with Expert Medical Coding and RCM Solutions

In the ever-evolving landscape of healthcare, ensuring streamlined revenue flow is crucial for providers. Our medical coding and revenue cycle management (RCM) solutions are meticulously designed to intertwine accurate medical coding with comprehensive financial processes. By aligning clinical documentation, coding precision, and billing workflows, we empower healthcare organizations to minimize claim errors, bolster compliance, and achieve faster reimbursements.
Understanding Medical Coding and RCM Solutions
Medical coding and RCM solutions are not just technical necessities; they are foundational elements that govern the financial lifecycle of healthcare services. This holistic approach encompasses:
- Clinical Documentation Review: Ensuring that every detail is accurately captured.
- ICD-10, CPT, and HCPCS Coding: Assigning codes that reflect diagnoses and procedures.
- Charge Capture and Validation: Confirming all billable services are accounted for.
- Claim Submission and Tracking: Sending claims systematically for timely processing.
- Denial Management and Appeals: Addressing and correcting rejected claims.
- Payment Posting and Reconciliation: Ensuring accurate recording of payments received.
By integrating these elements, we establish a streamlined workflow where coding accuracy directly enhances reimbursement efficiency.

Comprehensive Medical Coding Services
At the heart of our offering is a commitment to high-quality, accurate medical coding:
Accurate Medical Coding Services
Our team of certified coders ensures compliance with the latest coding standards, including:
- ICD-10-CM for diagnoses
- CPT for procedures
- HCPCS Level II for supplies and non-physician services
Charge Capture and Validation
We ensure that every eligible service is accurately captured and validated to prevent undercoding and missed revenue opportunities.
Claim Submission and Management
We prioritize clean claim submissions and maintain continuous tracking to guarantee timely responses from payers.
Denial Management and Appeals
Identifying patterns in denials enables us to rectify coding errors and file appeals, contributing to revenue recovery.
Payment Posting and A/R Follow-ups
By ensuring accurate payment posting and proactive accounts receivable management, we enhance cash flow and reduce outstanding balances.
The Importance of Medical Coding Accuracy
Accurate coding forms the backbone of an effective revenue cycle. Errors in coding can lead to several detrimental outcomes, including:
- Claim Denials and Rejections: Errors result in lost revenue and wasted resources.
- Delayed Reimbursements: Inaccuracies can hinder timely payments from insurers.
- Compliance and Audit Risks: Mistakes may lead to severe legal repercussions.
- Revenue Loss: The cumulative effect of errors can significantly impact a healthcare provider’s bottom line.
Our solutions ensure that accuracy is maintained at every step, safeguarding both revenue and compliance.
Benefits of Outsourcing Medical Coding and RCM Solutions
Opting to outsource your coding and RCM processes can provide numerous advantages:
- Access to Certified Professionals: Our team comprises seasoned coding experts, certified in their fields.
- Reduced Administrative Burdens: Outsourcing alleviates the workload, allowing staff to focus on patient care.
- Improved Claim Acceptance Rates: Our expertise results in fewer claim rejections.
- Faster Reimbursements: Efficient management accelerates payment cycles.
- Cost-Effectiveness: Outsourcing reduces operational costs significantly without compromising quality.
- Regulatory Compliance: We ensure alignment with CMS guidelines and payer requirements.
This shift allows healthcare providers to dedicate more time to the core mission of patient care, minimizing administrative distractions.
Our Streamlined Workflow
Our RCM workflow is designed to optimize every facet of the revenue cycle:
- Clinical Documentation Review: Ensure completeness and correctness.
- Accurate Code Assignment: Use the right codes to reflect services accurately.
- Charge Capture Validation: Confirm billable services before submission.
- Clean Claim Submission: Submit claims in a timely manner.
- Payment Posting and Reconciliation: Record payments accurately to protect revenue.
- Denial Analysis and Appeals: Correct errors and address denials proactively.
- Continuous Performance Monitoring: Regular check-ins to assess workflow efficiency.
Each of these steps is crafted to maximize revenue and minimize errors.
Who Can Benefit from Medical Coding and RCM Solutions?
Our comprehensive solutions are beneficial for a variety of healthcare entities, including:
- Hospitals and Health Systems
- Physician Practices
- Urgent Care Centers
- Specialty Clinics
- Behavioral Health Providers
- Medical Billing and RCM Companies
Large or small, our scalable solutions can adapt to each organization’s unique operational needs.
Why Choose ASP RCM Solutions?
Here’s why our clients trust us with their RCM needs:
- Expertise: Our team consists of certified medical coders with vast experience across multiple specialties.
- End-to-End RCM Services: We offer comprehensive solutions tailored to your needs.
- Compliance Assurance: Our workflows are designed to meet HIPAA standards, ensuring confidentiality.
- Proven Results: We have decreased denials and improved accounts receivable days.
- Transparent Reporting: Clients receive regular updates on their financial performance.
Our mission is to deliver accuracy, compliance, and sustainable revenue growth.
Frequently Asked Questions (FAQs)
What are medical coding RCM solutions?
These solutions integrate accurate coding with revenue cycle management to ensure efficient billing and expedient reimbursements.
How do coding errors affect RCM?
Errors can lead to claim denials, delayed payments, and compliance concerns, ultimately affecting revenue performance.
Do you support ICD-10, CPT, and HCPCS coding?
Absolutely! Our services encompass full coding support across all standard systems.
Can outsourcing improve cash flow?
Indeed, accurate coding and proactive RCM practices significantly enhance reimbursement timeliness and consistency.
Are your services compliant with applicable regulations?
Yes, we adhere to CMS guidelines, payer requirements, and HIPAA regulations.
Get Started with Our Medical Coding RCM Solutions
Partner with us for reliable medical coding and RCM solutions that ensure accuracy, compliance, and optimized financial performance. Optimize your revenue cycle and enhance reimbursements with assurance. Our tailored RCM solutions serve hospitals, clinics, and practices of every scale.
Patient Eligibility and Insurance Verification
Effective verification helps avoid claim rejections and clarifies financial responsibilities for patients.
Comprehensive Medical Coding and Charge Capture
Our certified coders guarantee precise coding to minimize errors and compliance issues.
Efficient Claim Submission and Management
Claims are submitted efficiently and tracked continuously for quicker responses from payers.
Accurate Payment Posting
We ensure correct payment postings and resolve discrepancies proactively to safeguard your revenue.
Denial Management and Appeals
Our experienced team analyzes denial trends and promptly submits appeals to recover missed revenue.
Accounts Receivable Follow-ups
Proactive follow-ups on A/R reduce outstanding balances and enhance cash flow.
Why Medical RCM Solutions Are Essential
In the absence of effective RCM, healthcare providers risk facing increased claim denials, delays in reimbursements, revenue leakage, compliance risks, and operational inefficiencies. Our medical RCM solutions address these challenges, creating a transparent and compliant billing workflow.
Final Thoughts
Outsourcing your RCM processes can transform your healthcare practice by reducing administrative burdens and enhancing revenue cycle efficiency. Experience financial stability and long-term growth by partnering with us for your medical coding and RCM needs. Let us help you streamline your revenue cycle and maximize your reimbursements effectively.
Consumer Services
Gift of Health This Valentine’s Day: GTA Fitness Gym Equipment

Valentine’s Day is traditionally associated with flowers, chocolates, and romantic gestures—but this year, why not give a gift that truly makes a lasting impact? Instead of a fleeting present, consider investing in the health and fitness of your loved ones. GTA Fitness, a leading provider of premium fitness equipment in Canada, is offering an exclusive Valentine’s Day Gym Equipment Sale. From essential home gym accessories to full workout setups, it’s the perfect opportunity to show care while promoting long-term wellness.
Why Fitness Equipment Makes the Perfect Valentine’s Day Gift
Gifting fitness equipment is thoughtful, practical, and impactful. Unlike consumable gifts that are quickly used or forgotten, gym equipment provides years of value. Choosing a gift that encourages exercise shows that you care about your loved one’s health, wellbeing, and lifestyle. Key benefits include:
-
Promotes Health and Longevity: Encourages consistent exercise for heart, joint, and muscle health
-
Builds Strength and Mobility: Helps improve overall fitness and reduce the risk of injuries
-
Motivation and Accountability: Having equipment at home makes workouts more accessible and consistent
-
Fun and Engagement: Couples or friends can workout together, making fitness a social and enjoyable activity
Whether your partner is a beginner, a fitness enthusiast, or someone who wants to start their journey, GTA Fitness offers a wide range of equipment that can meet all needs.

Top Gym Equipment to Consider for Valentine’s Day
-
Dumbbells and Weight Sets
Dumbbells are versatile, portable, and essential for full-body strength training. They allow for exercises like squats, lunges, presses, and rows, targeting multiple muscle groups. GTA Fitness offers premium dumbbell sets with adjustable weights to cater to both beginners and advanced lifters. Gifting a dumbbell set ensures your loved ones can perform a variety of workouts from the comfort of home. -
Workout Benches
Benches are a key component for many exercises such as bench presses, chest flys, step-ups, and seated presses. Adjustable benches provide additional versatility, allowing for flat, incline, and decline positions. GTA Fitness benches are ergonomically designed with durable frames and thick padding for comfort and safety. They serve as the foundation of a home gym, helping users target multiple muscle groups efficiently. -
Resistance Bands
Resistance bands are lightweight, portable, and extremely versatile. They help tone muscles, increase strength, and improve flexibility. From glute bridges and squats to arm exercises and stretching routines, resistance bands can be incorporated into countless workouts. GTA Fitness offers bands in various resistance levels, allowing for progressive training that adapts to the user’s strength and fitness level. -
Cardio Machines
Cardio machines like treadmills, ellipticals, and stationary bikes are excellent for cardiovascular health, endurance, and calorie burning. A treadmill allows for walking, jogging, or running indoors regardless of weather, while an elliptical provides a low-impact, full-body cardio experience. GTA Fitness cardio equipment is built for smooth operation, durability, and comfort, making it perfect for daily use at home or in professional setups. -
Full Home Gym Sets
For serious fitness enthusiasts, a complete home gym setup is the ultimate gift. These multi-functional machines allow a variety of exercises including presses, pulls, curls, and leg workouts—all in one compact design. GTA Fitness home gym systems combine strength training, cardio, and flexibility tools, creating a comprehensive solution for any fitness goal. These setups are ideal for couples who want to train together or anyone looking for a premium fitness solution.
Benefits of Gifting Gym Equipment
-
Encourages Consistent Workouts: Having equipment at home reduces excuses and promotes regular exercise
-
Supports Strength and Confidence: Strength training boosts self-esteem while improving overall body composition
-
Long-Term Value: Unlike short-lived gifts, gym equipment provides ongoing benefits for years
-
Promotes Shared Experiences: Couples or friends can workout together, making fitness fun and motivating
-
Adaptable for Any Fitness Level: Whether beginner or advanced, there’s equipment suitable for everyone
Tips for Choosing the Right Gym Equipment
-
Understand Their Fitness Goals: Determine whether your loved one is focused on strength, cardio, flexibility, or full-body training.
-
Measure Available Space: Ensure the equipment fits comfortably in their home or workout area.
-
Choose High-Quality Equipment: GTA Fitness products are durable, safe, and built to last.
-
Consider Usability: Select equipment that matches the user’s experience level, especially for beginners.
-
Balance Cost and Value: GTA Fitness offers a wide range of options that suit different budgets without compromising quality.
GTA Fitness Valentine’s Day Sale Highlights
-
Special offers on dumbbells, benches, resistance bands, and complete home gym configurations
-
Special offers on cardio machines suitable for couples and fitness enthusiasts
-
High-quality, durable, and safe equipment designed to last for years
-
Expert guidance and customer support to help select the right products
-
Flexible options for home gyms, small spaces, or professional setups
Tips to Make Your Fitness Gift Extra Special
-
Include a personalized workout plan or fitness challenge for motivation
-
Pair equipment with accessories like yoga mats, water bottles, or gloves
-
Write a motivational note or provide a fitness journal to track progress
-
Offer to join workouts together to make fitness a shared, fun experience
-
Create a themed gift package: combine resistance bands, dumbbells, and a workout guide for a thoughtful present
Why Fitness Gifts Make a Difference
Unlike traditional gifts, fitness equipment is meaningful and practical. It shows you care about your loved one’s health, goals, and long-term wellbeing. It also encourages habits that improve overall physical and mental health. Giving the gift of fitness this Valentine’s Day means investing in something that benefits your loved ones daily—far beyond a single occasion.
Conclusion
This Valentine’s Day, step away from ordinary gifts and give something that truly matters: the gift of health, strength, and motivation. GTA Fitness’ Valentine’s Day Gym Equipment Sale offers a wide range of high-quality products for all fitness levels. From dumbbells and benches to full home gym systems, these gifts empower your loved ones to stay active, strong, and inspired. Celebrate love in a meaningful way by supporting their fitness journey—because showing you care about their health is the ultimate expression of love.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom