health
Boost Your Immune System with These 10 Healthy Habits

Are you tired of getting sick every time the seasons change? Do you want to improve your overall health and well-being? Look no further! In this blog post, we’ll explore ten healthy habits that will help boost your immune system and keep you feeling great all year round. From eating nutrient-rich foods to getting enough sleep, these simple yet effective tips will have you on the path to a stronger immune system in no time. So put down that box of tissues and let’s get started!
Get Enough Fiber
If you’re looking to boost your immune system, adding more fiber to your diet may be one of the best ways to go. “Fiber is an immunoglobulin-binding agent that helps keep your gut healthy and regulates blood sugar levels,” says Tara Gidus, RDN, spokesperson for the American Dietetic Association. “It can also help reduce the risk of heart disease, cancer, and other chronic health conditions by promoting regularity and reducing inflammation.” Here are three ways you can get enough fiber in your diet:
1. Eat More Vegetables: One cup of chopped vegetables has about six grams of fiber. Including more servings of vegetables in your diet can help you reach your daily fiber goal.
2. Add Flaxseeds to Your Diet: Flaxseeds are a good source of plant-based omega-3 fatty acids and fiber. One tablespoon (15 grams) has about four grams of fiber. Add them to smoothies or salads for added texture and nutrition.
3. Swallow Probiotics Regularly: Good bacteria can help protect against bad bacteria in the gut, which can improve overall digestive health and support a strong immune system. Adding probiotics to your diet can help increase your intake of these beneficial microorganisms.
Eat Enough Omega-3s
One of the best ways to support your immune system is by eating foods high in Omega-3s. Omega-3s are essential fatty acids that play an important role in keeping your immune system functioning properly. The Mayo Clinic recommends that you eat at least 2 servings of fish per week, 1 serving of nuts or seeds per week, and a vegetable source of omega-3 every day.
Many people don’t get enough omega-3s from their diets because they don’t know how to prepare them or they think they need to avoid seafood altogether because of concerns about mercury levels. While large fish like tuna and swordfish are high in mercury, small fish like cod and panfish are a better choice because they contain lower levels of mercury. Also, try to eat organic fruits and vegetables whenever possible to get the highest level of antioxidants.
Get Enough Vitamin C
If you’re looking to bolster your body’s natural defenses against infection, adding more vitamin C to your diet may be a good place to start. This nutrient is essential for fighting off viruses, bacteria, and other infections. According to the National Institutes of Health (NIH), adults need about 75 mg of vitamin C daily.
To get the most benefit from this nutrient, try to incorporate it into your everyday routine in several ways. For example, eat fruits and vegetables that are high in vitamin C, or take supplements that include this mineral. Additionally, avoid drinking alcohol and smoking cigarettes because they can reduce your intake of this important vitamin.
Get Enough Iron
Iron is an essential mineral that helps make mitochondrial enzymes, neurotransmitters, and proteins. It’s also necessary for the production of hemoglobin and DNA. The National Institutes of Health recommend iron intake at 8 to 18 mg/day, but most Americans get less than half that amount. Here are five ways to boost your iron intake:
1. Eat red meat. Red meat contains heme — the element responsible for giving meat its color and flavor. Heme is also a good source of iron. A 3-ounce red meat steak has about 28 milligrams of iron, while a 3-ounce lamb chop has about 20 milligrams.
2. Include fortified foods in your diet. Many breakfast cereals, yogurt, juices, snack bars and energy bars are fortified with iron. Look for products that have 25 to 39 milligrams of iron per serving (one cup of cereal equals about 24 milligrams).
3. Add supplements to your regimen. Iron supplements are available as pills or as drops taken by mouth. The recommended daily dose is 18 to 24 milligrams (half a pill or one drop). However, because everyone absorbsIron differently, you may need to take more or less depending on your individual needs and health status
Get Plenty of Vitamin D
Looking to boost your immune system? Here are some healthy habits to start incorporating into your everyday routine:
1. Get plenty of vitamin D. Vitamin D is essential for maintaining a strong immune system. The best way to get your daily dose is through exposure to sunlight. If you can’t get outside, try supplementing with vitamin D3 supplements.
2. Eat healthy foods that contain antioxidants and vitamins C and E. These nutrients help protect the body against harmful toxins and foreign invaders.ioxidants like vitamin C can also help reduce the risk of various types of cancer, including lung cancer.
3. Drink plenty of water every day. Not only does drinking lots of water help keep your body hydrated, it also helps flush out toxins and waste products from your system.
4. Get a good night’s sleep every night. This is key for boosting immunity because it allows your body to recover from any wear and tear it experiences during the day.
Take Supplements Wisely
supplements can help to support your immune system, but it’s important to take them wisely. Too many supplements can actually do more harm than good, so make sure to talk with your healthcare provider before starting a supplement regimen. Here are some tips for taking supplements to support the health of your immune system:
-Choose safe and quality supplements. Make sure to research the ingredients in a given supplement before taking it. Some common ingredients that can interfere with the body’s natural defenses include gluten, dairy, soy, and yeast. If you have an autoimmune condition or any other type of health condition, be particularly careful about what supplements you take. Speak with your doctor or healthcare provider before starting any new supplement regimen.
-Start small. When starting a new supplement regimen, start with lower doses and work up gradually over time. This way you don’t risk overexposure to any one ingredient or group of ingredients in a supplement.
-Consider taking multiple supplements at once rather than all at once. This way you spread the dose out throughout the day and avoid having too much concentrated exposure to any one ingredient in a single capsule or tablet. It’s also easier to track how well each individual supplement is working if you take multiple smaller doses throughout the day instead of one large dose at bedtime.
-Regularly check for adverse effects and stop taking a supplement if you experience any unwanted side effects. Be especially vigilant if you’re trying a new formulation or
Conclusion
There is no question that our immune system plays a critical role in our overall health. By adopting healthy habits, we can help support and strengthen our immune system, which will help us stay healthy and fight off disease. Here are 10 healthy habits that you can start today to boost your immune system: 1) Eat a balanced diet high in fruits, vegetables, and whole grains. 2) Get enough exercise — both aerobic exercise and strength training workouts are great for supporting your immune system. 3) Take supplements such as vitamins C and E to increase your antioxidant levels. 4) Get plenty of sleep — sleeping well helps keep the body’s systems running smoothly, including the immune system. 5) Avoid stressors wherever possible — chronic stress can wreak havoc on the body’s delicate balance of hormones, leading to an increase in inflammation and other health problems. 6) Practice meditation or mindfulness every day to reduce anxiety and stress symptoms. 7) Use natural antimicrobial products like vinegar or essential oils at home or during the day (avoid using harsh chemicals around your home). 8 ) Make sure to get vaccinated against common infections; immunization programs have been shown to be very effective in boosting immunity 9 ) Consider taking probiotics daily 10 ) Use dietary supplements such as omega-3 fatty acids along with traditional medicinal herbs when needed
Care
Prenatal Multivitamin Gummies: A Guide for Expecting Mothers

Pregnancy is a time of great change for expecting mothers. During these nine months, proper nutrition becomes more important than ever, as it supports both the health of the mother and the development of the baby.
While a balanced diet is essential, it can be difficult for many expecting moms to get all the nutrients they need through food alone.
This is where prenatal vitamins, especially prenatal multivitamin gummies, play a critical role. These chewable supplements provide an easy, convenient, and effective way for mothers to ensure they are getting the necessary nutrients.

Why Prenatal Multivitamin Are a Game Changer for Expecting Moms
Prenatal multivitamin gummies offer a number of benefits that make them an appealing option for pregnant women. Not only are they a tasty alternative to traditional pills, but they also provide essential vitamins and minerals that are critical during pregnancy.
1. Convenience and Ease of Consumption
For many women, swallowing large pills can be difficult, particularly during pregnancy when nausea and morning sickness are common. Prenatal multivitamin gummies offer a much more palatable and enjoyable alternative.
With a variety of flavors and the ease of chewing rather than swallowing pills, these gummies help ensure that moms-to-be are more likely to stay consistent with their supplementation.
Additionally, their compact size and convenience make it easy to incorporate into daily routines. Whether at home or on-the-go, prenatal gummies can be taken at any time, ensuring moms don’t miss out on vital nutrients.
2. Rich Source of Essential Nutrients
Prenatal multivitamin gummies are formulated to support the nutritional needs of pregnant women. These gummies typically include vital vitamins and minerals such as:
- Folic Acid: This B-vitamin is one of the most important for a healthy pregnancy. Folic acid helps prevent birth defects of the brain and spine and is essential for fetal development.
- Iron: Pregnant women are at a higher risk of anemia due to increased blood volume. Iron helps support the increased demand for oxygen-carrying red blood cells and aids in preventing iron-deficiency anemia.
- Calcium: This mineral is necessary for the development of the baby’s bones and teeth. It additionally aids in preserving the mother’s bone health throughout pregnancy.
- Vitamin D: Vitamin D supports the immune system and helps the body absorb calcium more efficiently, which is critical for both the mother and the baby.
- Iodine: Iodine is crucial for proper thyroid function and plays a key role in the baby’s brain development.
Many prenatal gummy supplements also include other beneficial nutrients such as Vitamin A, Vitamin C, and Zinc, all of which play a part in immune function, skin health, and overall wellness for both mom and baby.
3. Better Absorption and Less Risk of Stomach Upset
Unlike traditional prenatal pills, which can be tough on a sensitive stomach, prenatal multivitamin gummies are generally easier to digest and less likely to cause stomach upset.
Many pregnant women experience nausea, heartburn, or indigestion, especially during the first trimester. Gummies tend to be gentler on the digestive system, allowing moms to get the essential nutrients without the discomfort associated with pill form.
Moreover, since these vitamins are in a chewable form, they are absorbed more quickly into the bloodstream, leading to faster and potentially more efficient nutrient delivery to both mother and baby.
4. Improved Adherence to Prenatal Supplementation
One of the challenges many expecting mothers face is maintaining consistency with their prenatal supplementation. Studies have shown that when prenatal vitamins are in a more appealing form, like gummies, women are more likely to follow their supplementation schedule.
The tasty flavors make it easier for pregnant women to take their daily dose without forgetting or feeling overwhelmed by the process.
This consistent adherence helps ensure that both the mother and baby receive the required nutrients every day, supporting healthy growth and development throughout the pregnancy.
The Role of Prenatal Multivitamin Gummies in Supporting a Healthy Pregnancy
Prenatal multivitamin gummies play an essential role in filling nutritional gaps that may exist in the diet of an expecting mom. While a well-balanced diet should ideally provide all the necessary nutrients, pregnancy increases a woman’s nutritional requirements.
Often, women experience food aversions or cravings, making it difficult to maintain a balanced diet. These nutritional gaps can be addressed with the help of prenatal multivitamin gummies, ensuring that mom and baby have the vitamins and minerals they need.
Furthermore, supplements like prenatal vitamins have been shown to help reduce the risk of pregnancy complications, including preterm labor and low birth weight.
Consuming the right combination of nutrients during pregnancy also helps optimize fetal development, ensuring babies are born healthy and strong.
How Prenatal Multivitamin Gummies Help With Specific Pregnancy Symptoms
Pregnancy can bring with it a variety of symptoms, some of which can be mitigated with proper supplementation. Prenatal multivitamin gummies, with their specific formulation of vitamins and minerals, are designed to help with the following common pregnancy concerns:
- Morning Sickness: Prenatal gummies are typically easier on the stomach and less likely to induce nausea compared to traditional tablets. Vitamin B6, which is commonly found in these gummies, is known to help reduce nausea, making it a popular remedy for morning sickness.
- Fatigue: The increased iron content in prenatal multivitamin gummies can help combat fatigue caused by low iron levels. Iron is essential for producing red blood cells that carry oxygen to both the mother and baby, helping moms-to-be feel more energized.
- Immune Support: Pregnancy often weakens the immune system, and supplements like Vitamin C and Zinc found in prenatal multivitamins help bolster the immune system. These vitamins support the body in fighting off infections and maintaining overall health during pregnancy.
Are Prenatal Multivitamin Gummies as Effective as Traditional Pills?
Many expecting mothers may wonder whether prenatal gummies are as effective as traditional pill supplements. The answer largely depends on the specific formulation of the product.
While both forms of supplementation are effective, gummies tend to offer a slightly higher level of bioavailability, meaning that the body absorbs them faster and more efficiently.
However, it is important to choose a high-quality prenatal gummy that contains the right balance of nutrients. Not all gummy supplements are created equal, so it’s important to consult with a healthcare provider to ensure the product meets the specific nutritional needs of the mother and baby.
Conclusion
Prenatal multivitamin gummies are an excellent option for expecting mothers seeking a convenient, gentle, and effective way to support their pregnancy health.
With essential vitamins and minerals like folic acid, iron, calcium, and Vitamin D, these gummies provide a vital source of nutrients for both the mother and the developing baby.
They are particularly beneficial for women who may struggle with traditional prenatal pills or those who experience nausea during pregnancy.
By making it easier to stay consistent with supplementation, prenatal multivitamin gummies help ensure that the mother’s nutritional needs are met, supporting healthy fetal development and a smoother pregnancy journey.
For expecting mothers, choosing high-quality prenatal multivitamin gummies can truly make a difference in how they feel and how their pregnancy progresses, providing peace of mind and a healthier start for both mom and baby.
Care
Leukoplakia: Causes, Symptoms, and Treatment for Oral Health

White patches inside the mouth can be worrying, especially when they appear unexpectedly or refuse to go away. Among the most common causes of such patches is a condition known as leukopakia. While it is often harmless, leukoplakia can occasionally signal early signs of more serious problems, making awareness and early detection essential.
Understanding what leukoplakia looks like, why it develops, and how it is treated empowers individuals to take charge of their oral health. This guide walks you through the key facts, symptoms and treatment options, offering clarity and confidence for those who may be noticing unusual changes in their mouth.
What Is Leukopakia?
Leukoplakia refers to thickened white or grey patches that form inside the mouth due to excessive cell growth, often triggered by long-term irritation. These patches may appear on the gums, inner cheeks, tongue, or roof of the mouth. While many cases are harmless, some require monitoring to ensure no further complications develop. Early detection is important because changes can sometimes indicate underlying issues.
Types of leukoplakia:
- Ordinary leukoplakia: Commonly linked to tobacco use and continual irritation.
- Hairy leukoplakia: Associated with viral infections and seen more frequently in individuals with weakened immune systems.
Identifying leukoplakia early helps ensure abnormalities are evaluated promptly and managed before they progress.

What Do Leukoplakia Patches Look Like?
Leukoplakia patches usually appear as uneven, slightly raised areas that feel rough and range in color from white to grey. They cannot be scraped off, which helps distinguish them from conditions like oral thrush. Although generally painless, some people may notice mild sensitivity or irritation, especially when consuming hot or spicy foods. Sudden changes in appearance should be taken seriously.
Warning signs that require urgent evaluation:
- Patches turning red or darkening
- Rapid growth in size
- Increasing discomfort or sensitivity
These changes are often first spotted during brushing or routine dental visits, highlighting the importance of regular check-ups with a dentist or a hygienist in Chichester.
Common Causes & Risk Factors
Leukopakia can be triggered by several factors. Some of the most common include:
Lifestyle-related causes
- Tobacco use: Smoking or chewing tobacco remains the most significant cause, responsible for the majority of diagnosed cases.
- Excessive alcohol consumption: Alcohol irritates the oral tissues and magnifies the effects of smoking when combined.
Irritation-related causes
- Rough or sharp teeth rubbing against the inside of the mouth
- Poorly fitted dentures
- Chronic cheek or tongue biting
Medical and biological factors
- Viral infections such as Epstein–Barr virus
- Weakened immune systems
- Ageing and prolonged exposure to irritants
In some instances, individuals discover leukoplakia when visiting an emergency dentist in Chichester due to pain, bleeding or sudden irritation, even though these signs are not always directly caused by the patches themselves.
Diagnosis: How Professionals Identify Leukoplakia
Diagnosing leukoplakia usually starts with a clinical examination, where a dental professional assesses the affected area, reviews medical history, and asks about habits such as smoking or alcohol use. If a patch persists for more than two weeks, further investigation is required to determine the cause. A biopsy is commonly recommended to rule out precancerous changes, involving the removal of a small tissue sample for laboratory analysis. This quick, straightforward procedure helps identify whether the cells show signs of concern.
Additional diagnostic steps may include:
- Extra testing for hairy leukoplakia, especially if a viral condition is suspected
- Imaging or specialist assessment when needed
- Close monitoring of changes in size, texture, or color
Early diagnosis ensures that any potentially harmful developments are addressed promptly. Routine check-ups with a dental professional or a hygienist in Chichester also support long-term monitoring and early detection of new or evolving patches.
Treatment Options
1. Lifestyle and Habit Changes
The first step in managing leukoplakia often involves removing the source of irritation. This may include:
- Stopping smoking or chewing tobacco
- Reducing alcohol intake
- Improving daily oral hygiene practices
For many people, simply eliminating the irritant leads to noticeable improvement or complete resolution of the patches.
2. Dental and Medical Interventions
If leukoplakia is caused by irritation from a sharp tooth or poorly fitting denture, adjustments or replacements may be needed. Hairy leukoplakia may require medication, especially when linked to viral or immune issues. Sudden discomfort, bleeding, or rapid changes should prompt a visit to an emergency dentist in Chichester.
3. Surgical Treatments
If a biopsy reveals dysplasia or if the patches become particularly large or concerning, removal may be recommended. This can be done through:
- Laser therapy
- Cryotherapy (freezing the tissue)
- Traditional surgical excision
These procedures are typically quick and carried out under local anaesthesia, offering reassurance and protection against further risk.
Can Leukoplakia Turn Into Cancer?
Although most cases of leukoplakia remain harmless, a small number can develop into oral cancer over time. Factors that increase this risk include:
- Red patches mixed with white (erythroplakia)
- Rapid growth of the patch
- Persistent soreness or pain
- A long history of smoking and drinking
This is why regular monitoring is essential. With professional guidance and periodic check-ups, any suspicious changes can be caught early, significantly reducing long-term risk.
Prevention Tips
Good oral health habits are key to lowering your risk of developing leukoplakia. Consider the following preventive strategies:
| Preventive Action | Benefit |
| Quit smoking/tobacco | Reduces irritation and cancer risk |
| Limit alcohol use | Protects oral tissues |
| Address dental issues promptly | Prevents chronic friction |
| Maintain strong oral hygiene | Promotes healthier tissue |
| Attend regular dental check-ups | Ensures early detection |
A balanced diet, hydration and regular cleanings can further help maintain healthy oral tissues and reduce irritation.
When to See a Dental Professional
You should seek professional advice if:
- A white or grey patch lasts longer than two weeks
- There is persistent pain, discomfort or bleeding
- The patch changes shape, size or color
- You are a long-term smoker or drinker and notice new symptoms
Early assessment ensures greater peace of mind and more effective treatment options.
Conclusion
Leukoplakia may be a common condition, but paying attention to changes in your oral health is crucial. While most cases remain harmless, staying aware of symptoms, eliminating risk factors and seeking timely professional advice can significantly reduce complications. With the support of experienced dental professionals and proactive habits, you can maintain long-term oral health and confidence. For reliable care and regular check-ups, you can always count on Chichester to guide you toward better oral health and peace of mind.
Care
Enhance Your Career with the OSHA Industrial Safety Course
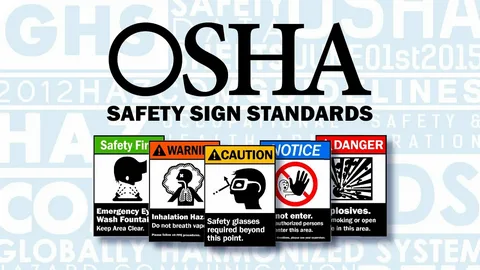
Introduction
Safety at work is a need in the contemporary industrial and construction industries which are experiencing rapid expansion. The manufacturing sectors also require skilled workers who are conversant with the international safety measures as well as preventing accidents before they occur. This is whereby the OSHA Industrial Safety Course in Rawalpindi comes in.
United College of Technology is pleased to provide a single and career oriented OSHA course in Rawalpindi that is intended to incorporate the current industry demand and global safety measures. This course is best suited to students, individuals, and organizations that would wish to enhance workplace safety and compliance.
What Is OSHA and Why Is It Important?
OSHA is an acronym of Occupational Safety and Health Administration, which is an internationally acclaimed author that establishes the safety standards in the places of work. OSHA guidelines have been used to minimize workplace hazards, injuries, and in favor of a robust safety culture in industries like:
- Construction
- Manufacturing
- Oil & Gas
- Engineering
- Power Plants
- Factories and Warehouses
Students can obtain real knowledge about rules of industrial safety which are recognized in the world by attending an OSHA course in Rawalpindi.

OSHA Industrial Safety Course in Rawalpindi – Course Overview.
United College of Technology provides the OSHA Industrial Safety Course in Rawalpindi that concentrates on the practical aspects of safety concerns in an industrial setting. The course involves both theoretical and practical studies to make sure that everything is understood.
Key Learning Areas Include:
- Detection of hazards in industries.
- Risk evaluation and management.
- The prevention of accidents at work.
- Safety signs and symbols
- Personal Protective Equipment (PPE).
- Fire and emergency response.
- Safety of electricity and mechanical.
- Standards of health and environmental safety.
The course is an OSHA in Rawalpindi course which is appropriate to both the novice and the already established professionals in need of certification regarding safety.
Why United College of Technology to take OSHA Course in Rawalpindi?
The selection of the appropriate institute is of important concern to quality education and progress of career. United College of technology is among the most reputable technical colleges that provide professional courses in terms of safety in the city of Rawalpindi.
The advantages of studying at United College of Technology are as follows:
- Well trained, professional teachers.
- Industry-relevant curriculum
- On-the-job training model.
- Affordable course fees
- Recognized OSHA certification.
- Career guidance and support
We would like to have qualified safety professionals who are capable of fulfilling both local and international industry requirements.
Career Scope Following OSHA Industrial Safety Course.
On finishing the OSHA Industrial Safety Course in Rawalpindi, students have an opportunity to take different jobs in the sphere of safety in Pakistan and other countries.
Career Opportunities It includes:
- Safety Officer
- Supervisor of industrial safety.
- HSE Officer
- Site Safety Inspector
- Safety Coordinator
- Health and Safety Manager (experienced).
The OSHA-certified professionals are in high demand particularly in the construction work, factories, and multinational enterprises.
Who Can enroll in OSHA Course in Rawalpindi?
The course is an OSHA program in Rawalpindi that is accessible to a large group of learners, and they include:
- Fresh students
- Diploma holders
- Engineers
- Site supervisors
- Technicians
- Factory workers
- Safety professionals
There is no higher education level needed and this is why it is easy to use and accessible to any person interested in workplace safety.
Experiential Training and Industry-Based Learning.
We are of the opinion that theory is not as valuable as practice is at United College of Technology. The OSHA Industrial Safety Course of Rawalpindi has real life case studies, safety drills and analysis of hazards to equip the students with the real work conditions.
Such practical method enables students to be able to use safety regulations with a lot of confidence in their job sites and industrial workplaces.
The importance of OSHA Certification in Pakistan and Europe.
The employers nowadays are attracted to the candidates who have professional safety certification. An OSHA course in Rawalpindi is not only one that is going to enhance your knowledge of safety but also improve your CV and employment opportunities.
The certification of OSHA demonstrates that you:
- Know the international standards of safety.
- Can reduce workplace risks
- Trained to deal with emergencies.
- Appreciate health and safety compliance.
- That would make you a valuable investment in any company.
Conclusion
The industrial Safety Course provided by the OSHA in Rawalpindi by United College of Technology is a good chance to have a good career in industrial and workplace safety. As more industry expands, the need to have professional safety workers is more than ever.
Studying this OSHA course in Rawalpindi you obtain internationally accepted knowledge, practical skills and get better employment opportunities not only in Pakistan but also in the abroad. United College of Technology is the place to begin in case you are serious about safety, professionalism and career development.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom