health
Benefits of Letting Go of Resentment

In a world that often fosters grudges and nurtures resentments, forgiveness emerges as a powerful force that can bring about profound personal and societal change. The act of forgiving is not only an act of kindness but also a transformative process that can have far-reaching benefits. Let’s delve into why forgiveness matters and explore the positive impact it can have on our lives.
Forgiveness is a conscious decision to release feelings of anger, bitterness, and resentment towards someone who has caused us pain. It is not about condoning or forgetting the hurtful actions, but rather about freeing ourselves from the emotional burden that weighs us down.
Psychological research has shown that practicing forgiveness can have a myriad of benefits for our mental well-being. When we hold onto grudges and resentments, we subject ourselves to chronic stress, which can lead to a range of negative health outcomes, including increased anxiety and depression. By choosing forgiveness, we reduce stress levels, enhance our emotional resilience, and experience an improved sense of overall well-being.
Moreover, forgiveness has been linked to better physical health outcomes. The act of letting go of resentment can have a positive impact on our physiological responses, leading to lower blood pressure, reduced heart rate, and improved immune system functioning. By forgiving, we create a state of inner harmony that promotes healing and fosters better physical health.
One of the most significant benefits of forgiveness lies in its ability to repair and nurture relationships. When we hold onto grudges, we create barriers and distance between ourselves and others. However, forgiveness has the power to break down those walls and rebuild trust, fostering stronger connections and deeper understanding. It opens the door to reconciliation, allowing both parties to heal and grow from their shared experience.
In addition to its personal benefits, forgiveness also has a broader societal impact. In a world often divided by conflict and animosity, forgiveness acts as a catalyst for social healing and reconciliation. It has the power to break cycles of violence, bridge divides, and promote empathy and understanding. By choosing forgiveness, we contribute to a more compassionate and harmonious society.
But forgiveness is not always an easy path to tread. It requires courage, introspection, and self-reflection. Sometimes, the wounds inflicted are deep, and the journey towards forgiveness can be long and arduous. It is essential to acknowledge the pain caused, validate our emotions, and seek support from loved ones or professionals who can help guide us through the process.
In the face of injustice, forgiveness does not mean turning a blind eye or accepting wrongdoing. It is about finding a balance between seeking justice and letting go of personal resentment. Forgiveness empowers us to advocate for change and pursue justice while freeing ourselves from the emotional burden that hinders our personal growth.
In conclusion, forgiveness matters because it allows us to break free from the chains of anger, resentment, and bitterness. It enhances our mental and physical well-being, strengthens relationships, and fosters social healing. The act of forgiveness is a powerful tool that has the potential to transform lives and create a more compassionate and empathetic world.
So, let us embrace forgiveness as a force for personal and societal change. By choosing forgiveness, we take a courageous step towards healing, growth, and the creation of a brighter future.
Beauty Fitness
Restoring Facial Volume: Dermal Fillers and Their Longevity

If you’re noticing hollow cheeks, deeper smile lines, or sunken temples, you’re experiencing what millions face as they age: facial volume loss. While these changes are natural, they can make you look tired or older than you feel. The good news? Modern dermal filler treatments offer a safe, effective solution to restore youthful volume without surgery. But one question remains top of mind for most people considering treatment: how long will the results actually last?
Understanding the longevity of facial volume loss treatments is essential for planning your aesthetic journey and budget. Whether you’re exploring options for facial volume loss Boca Raton or simply researching, this comprehensive guide will help you understand what to expect from your investment.

Understanding Facial Volume Loss
It is a natural part of aging, as the fat pads beneath our skin diminish, and collagen production slows. This process typically begins in our mid-to-late twenties and accelerates as we enter our thirties and beyond.
Several factors contribute to facial volume loss, including genetics, sun exposure, weight fluctuations, stress, and lifestyle habits like smoking. The loss doesn’t happen uniformly across the face. Common areas affected include the cheeks, temples, under-eye hollows, lips, chin, and jawline. These changes can create a gaunt appearance, deepen wrinkles, and alter facial contours that once defined your youthful look.
The impact goes beyond aesthetics. Many people report feeling less confident or concerned that their appearance doesn’t match how vibrant they feel inside. This disconnect drives many to seek treatments that can restore their natural volume and refresh their appearance.
Dermal Fillers: The Leading Solution
Dermal fillers have emerged as the gold standard for treating facial volume loss. These injectable gel-like substances, most commonly made from hyaluronic acid, replenish lost volume beneath the skin’s surface. Hyaluronic acid is a naturally occurring substance in the body that helps maintain skin hydration and plumpness.
When strategically injected by a skilled practitioner, dermal fillers can restore fullness to hollow areas, smooth wrinkles and folds, enhance facial contours, and create overall facial harmony. The procedure is minimally invasive, involves minimal recovery time, and delivers noticeable results right away—enhancing further as mild swelling gradually resolves.
Popular filler brands used for facial volume restoration include Juvederm, Restylane, and Sculptra, each formulated for specific areas and treatment goals. The choice of filler depends on the treatment area, the desired outcome, and the individual patient’s needs.
Duration of Results: What to Expect
The longevity of dermal filler results varies based on several factors, but most patients can expect their results to last between 6 and 18 months. However, this timeline isn’t one-size-fits-all.
Treatment Area Impact
Different areas of the face experience varying levels of movement and muscle activity, which affects how long fillers last. Lips typically see results lasting 6 to 9 months due to constant movement from talking, eating, and facial expressions. Cheeks and mid-face areas usually maintain results for 9 to 12 months, while under-eye fillers can last 9 to 12 months or longer. Chin and jawline fillers often provide the longest-lasting results, typically 12 to 18 months, as these areas experience less dynamic movement.
Filler Type Matters
Different formulations have varying durations. Traditional hyaluronic acid fillers last 6 to 12 months on average. More robust formulations designed for deeper volumization can last 12 to 18 months. Biostimulatory fillers such as Sculptra operate by encouraging collagen production and can yield results that last for 2 years or longer.
Individual Factors
Your body’s unique metabolism plays a significant role in how quickly filler breaks down. Those with faster metabolisms may find their results fade more quickly. Age also matters, as younger patients with better skin elasticity may experience longer-lasting results. Lifestyle factors, including exercise intensity, sun exposure, and smoking, can all affect longevity. Additionally, first-time patients may notice that their initial treatment doesn’t last as long, while maintenance treatments often do.
Maximizing Your Results
While the natural breakdown of fillers is inevitable, you can take steps to extend your results and maintain your refreshed appearance.
Immediate Aftercare
Following your treatment, avoid strenuous exercise for 24 to 48 hours, as elevated heart rate and blood pressure can increase swelling. Stay away from excessive heat, including saunas, hot tubs, and direct sunlight. Don’t massage or apply pressure to treated areas unless your provider instructs you to do so. Keep your head raised while sleeping for the initial nights to reduce swelling.
Long-Term Maintenance
Protect your investment by using broad-spectrum SPF daily, as sun damage accelerates the breakdown of fillers and contributes to further volume loss. Keep a regular skincare regimen using high-quality products that promote skin wellness.
Stay well-hydrated, as hyaluronic acid fillers attract and retain water. Consider scheduling maintenance appointments before your results completely fade for optimal ongoing results.
Follow-Up Treatments
Most providers recommend touch-up appointments every 9 to 12 months to maintain your desired look. These maintenance sessions typically require less product than initial treatments, making them more cost-effective over time.
Choosing the Right Provider in Boca Raton
The skill and experience of your injector significantly impact both the quality and longevity of your results. When seeking treatment for facial volume loss in Boca Raton, prioritize providers with proper credentials, including board certification and specialized training in aesthetic injectables.
Look for practitioners who take a personalized approach, carefully assessing your unique facial anatomy and creating customized treatment plans. Review before-and-after photos of actual patients to evaluate their aesthetic style and skill level. A provider who stays current with the latest techniques and products can offer you the most advanced, effective treatments available.
During your consultation, a qualified provider should thoroughly discuss your goals, explain which fillers are best suited to your needs, set realistic expectations for results and longevity, and create a comprehensive treatment plan that may include multiple areas for balanced facial rejuvenation.
Conclusion
Understanding how long facial volume loss treatment results last helps you make informed decisions about your aesthetic journey. While most dermal filler results last between 6 and 18 months, depending on various factors, the confidence and refreshed appearance they provide can be truly transformative.
The key to maximizing your investment lies in choosing an experienced provider, following proper aftercare instructions, and maintaining your results with scheduled touch-up treatments. With the right approach, you can enjoy natural-looking, age-defying results that help you look and feel your best.
Care
Tirzepatide vs Semaglutide: Better Option for Metabolic Health?
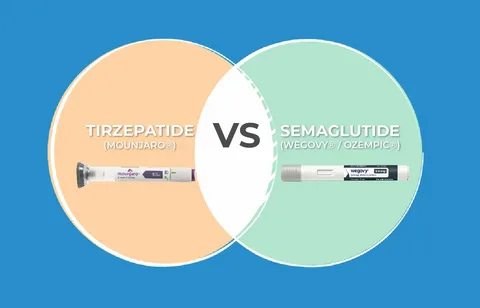
The rising prevalence of metabolic disorders has led to increased demand for effective treatment options. Two medications have emerged as frontrunners in addressing metabolic health concerns: which is better tirzepatide or semaglutide. Both have shown remarkable results in clinical settings, but understanding which is better, tirzepatide or semaglutide, requires examining their unique characteristics and benefits. Recent research suggests that tirzepatide may offer greater weight-loss potential due to its dual-agonist mechanism.
Semaglutide, however, remains a well-established option with extensive clinical data supporting its effectiveness. Patient tolerance, dosage requirements, and long-term goals can also influence which medication is more suitable. Ultimately, choosing between tirzepatide and semaglutide depends on personalized medical guidance and individual health needs.

Understanding the Medications
What is Semaglutide?
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that has revolutionized the treatment of metabolic health. Originally approved for type 2 diabetes management, it works by mimicking the GLP-1 hormone that your body naturally produces. This medication enhances insulin secretion, slows gastric emptying, and reduces appetite, providing a comprehensive approach to improving metabolic health.
What is Tirzepatide?
Tirzepatide represents the next generation of metabolic medications. Unlike semaglutide, it acts as a dual agonist, activating both the GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors. This dual-action mechanism provides a more comprehensive metabolic response, offering enhanced benefits for those struggling with weight management and blood sugar control.
Key Differences in Mechanism
The fundamental distinction lies in their receptor activity. While semaglutide targets GLP-1 receptors exclusively, tirzepatide’s dual-receptor approach activates both the GLP-1 and GIP pathways. This dual mechanism may explain tirzepatide’s potentially superior performance in certain metabolic outcomes, though both medications demonstrate significant efficacy.
Effectiveness for Weight Loss
Clinical trials have provided compelling data on both medications’ weight loss capabilities. Studies show that semaglutide users typically experience weight reduction of approximately 15-17% of their initial body weight over 68 weeks. These results have positioned semaglutide as a powerful tool for weight management.
Tirzepatide has demonstrated even more impressive results in clinical trials. Patients using the highest approved dose achieved an average weight loss of approximately 20-22% of their starting weight. The SURMOUNT trials revealed that tirzepatide consistently outperformed placebo and showed superior weight reduction compared to similar medications in head-to-head comparisons.
Impact on Blood Sugar Control
Both medications excel at improving glycemic control in patients with type 2 diabetes. Semaglutide successfully reduces HbA1c levels, an important indicator of long-term blood sugar regulation, by approximately 1.5-2%. This reduction represents a significant improvement for individuals struggling with glucose management.
Tirzepatide’s dual-action mechanism offers slightly superior blood sugar control. Clinical data suggest HbA1c reductions of approximately 2-2.5%, potentially providing an edge for patients requiring more aggressive glucose management. The medication’s ability to stimulate insulin release while suppressing glucagon secretion creates a powerful combination for metabolic regulation.
Metabolic Health Benefits Beyond Weight Loss
Cardiovascular Improvements
Both medications have shown promise in supporting cardiovascular health. Semaglutide has demonstrated cardiovascular benefits in clinical trials, including reduced risk of major cardiovascular events in high-risk patients. These benefits extend beyond simple weight loss, suggesting direct protective effects on the cardiovascular system.
Insulin Sensitivity
Improved insulin sensitivity is a crucial marker of metabolic health. Both tirzepatide and semaglutide enhance insulin sensitivity, addressing a fundamental issue in metabolic dysfunction. Tirzepatide’s dual mechanism may provide additional advantages in this area, though both medications show meaningful improvements.
Overall Metabolic Markers
Patients using either medication often experience improvements in multiple metabolic markers, including triglycerides, cholesterol levels, and blood pressure. These comprehensive benefits suggest that both medications address metabolic health holistically rather than targeting isolated symptoms.
Practical Considerations
Dosing and Administration
Both medications are administered via weekly subcutaneous injections, making them convenient for long-term use. Semaglutide is available in pre-filled pens with straightforward dosing escalation protocols. Tirzepatide follows a similar administration method with its own titration schedule designed to optimize results while allowing the body to adjust.
Accessibility and Cost
Who Should Choose Which?
Determining which is better, tirzepatide or semaglutide, depends on individual circumstances. Patients requiring maximum weight loss may benefit more from tirzepatide’s superior weight-loss profile. Those with well-controlled diabetes seeking moderate weight loss may find semaglutide perfectly adequate.
Medical history, current medications, and specific metabolic goals should guide decision-making. Some patients may respond better to one medication than the other, depending on their unique physiology and health status.
Conclusion
Both tirzepatide and semaglutide represent powerful tools for improving metabolic health. While tirzepatide shows slightly superior results in weight loss and blood sugar control due to its dual-action mechanism, semaglutide remains highly effective with a longer track record of use.
The question of which is better, tirzepatide or semaglutide, ultimately depends on individual needs, goals, and circumstances. Consultation with a qualified healthcare provider is essential to determine the most appropriate option for your specific metabolic health journey.
Care
Right Family Dentist in Cypress, TX: A Comprehensive Guide

Choosing a dentist for your family is a significant decision, more personal than many realize. It goes beyond merely booking dental cleanings; it’s about entrusting someone with your comfort, health, and often your confidence. In a close-knit community like Cypress, TX, that trust holds even greater importance. Families seek care that feels familiar, consistent, and genuinely focused on their long-term well-being.

The Importance of Oral Health
Oral health impacts daily life in countless ways that often go unnoticed. It shapes how you eat, how you speak, and influences your self-esteem in social situations. When dental care is rushed or inconsistent, small issues can escalate into painful problems. Many families in Cypress prioritize proactive dental care, aiming for a preventive approach rather than a reactive one.
For those seeking a reliable practice that can accommodate various ages and stages, Cypress family dental care offers a unique solution. This comprehensive approach fosters continuity. Instead of hopping between different offices, families can develop relationships with a team that understands their specific history and priorities. This familiarity leads to informed decisions, fewer emergency situations, and a more streamlined experience.
What Comprehensive Dental Care Looks Like
Comprehensive dentistry is rooted in the understanding that no two patients are identical. This approach integrates prevention, education, treatment, and long-term planning into a cohesive system. Instead of waiting for discomfort to arise, dentists prioritize maintaining health and preventing future issues.
Preventive care lays the foundation for everything. Regular check-ups and cleanings facilitate early detection of problems like decay and gum disease. These visits also allow patients the opportunity to ask questions and learn better habits, as minor adjustments to daily routines can result in a lifetime of dental health.
When therapeutic intervention is necessary, restorative dentistry comes into play. Treatments such as fillings, crowns, and root canal therapy restore lost tooth structures. Many patients find that modern procedures are far more routine and less painful than they had anticipated.
Cosmetic care plays its part, as well. Treatments like whitening, bonding, and veneers can revitalize smiles and boost self-confidence. However, they also contribute to long-term oral health by improving the structure and cleanliness of teeth.
While some patients might require orthodontic intervention for issues related to teeth spacing or bite, the coordination of these services within a single practice offers considerable benefits. This integration helps families manage their dental care more efficiently.
Why Family Dentistry Matters in Cypress, TX
Cypress continues to grow, attracting families who value strong schools, safe neighborhoods, and reliable healthcare. This growth generates a demand for consistent dental providers who focus on long-term care rather than quick fixes.
Family dentistry simplifies life for parents. Appointments can be easily coordinated, medical records remain consolidated, and overall care feels more cohesive. Parents appreciate not needing to repeat their children’s medical histories at every visit. Children, in turn, benefit from regularly seeing the same friendly faces.
For adults, this continuity translates to better health outcomes. A dentist familiar with your past treatments can detect changes early and tailor care to fit your individual needs. This long-term perspective often prevents the need for more extensive interventions down the line.
Just as crucial is the comfort that comes with familiarity. Entering an office where the staff recognizes you increases the likelihood of a positive experience, making routine visits manageable rather than anxiety-inducing.
Supporting Children and Creating Healthy Foundations
Early dental treatment sets the stage for a child’s lifelong relationship with oral health. When children feel comfortable in the dental office, they are more likely to maintain good habits as adults. Regular check-ups allow dentists to monitor tooth development and jaw growth, identifying issues related to crowding or bites before they become significant problems.
Preventive measures such as sealants and fluoride treatments provide added layers of protection. Sealants guard molars against decay, while fluoride strengthens enamel. These small steps can prevent years of dental issues down the road.
Creating a welcoming atmosphere is crucial for children’s visits. Trust is established when kids feel respected and heard, making them active participants in their own care rather than passive recipients of treatment.
Navigating Teen Years and Changing Dental Needs
The teenage years can present unique challenges for oral health. Hormonal changes may impact gum health, and busy lifestyles can lead to disrupted brushing routines. This stage is also when many families start considering orthodontic options.
Orthodontic care is not just about aesthetics; it offers functional benefits, too. Straightening teeth can improve bite function and make daily cleaning simpler, boosting overall confidence. Dentists collaborate with families to explore the best options, whether that’s traditional braces or clear aligners while monitoring wisdom tooth development.
Teen dental care emphasizes more than just appearance; it encourages personal responsibility and forms healthy habits that will last a lifetime.
Adult Dental Care: Maintenance and Restoration
For adults, maintenance and restorative procedures become the primary focus. Balancing work, family, and personal life can make it easy to postpone dental appointments, yet neglecting minor issues often leads to more significant problems.
Routine check-ups enable the early detection of decay and gum disease, both of which have significant implications for overall health. Neglected gum health can lead to tooth loss and has been linked to other serious health conditions.
Restorative procedures, such as crowns, implants, and bridges, not only restore functionality but also enhance comfort. Many adults find that enhancing their dental work can significantly improve their quality of life.
Cosmetic treatments like bonding and whitening can also boost confidence, creating positive effects in both personal and professional spheres.
Dental Care for Seniors: Emphasizing Comfort and Function
As individuals age, their oral health needs become more complex. Factors like enamel wear, gum recession, and changes in saliva production require age-specific care strategies.
Dentists monitor for issues such as dry mouth, gum disease, and oral cancers while maintaining existing restorations to ensure comfort and proper function. These considerations directly influence nutrition, speech, and overall wellness.
Education and guidance remain vital for seniors. Dentists provide advice on hydration, diet, and at-home care routines that support oral health, making many age-related challenges manageable.
Staying with a trusted dental team can offer peace of mind for seniors. Long-term relationships foster trust, reducing anxiety about ongoing care.
Practical Ways to Maintain Your Family’s Oral Health
Building Consistent Routines: Encourage brushing twice daily with fluoride toothpaste and daily flossing. Consistency often trumps perfection.
Scheduling Regular Visits: Most families benefit from biannual check-ups, allowing dentists to conduct thorough cleanings and catch issues before they escalate.
Making Healthy Food Choices: Reducing sugary snacks and acidic beverages can lower the risk of cavities. Prioritizing water, fresh produce, and calcium-rich foods strengthens teeth and gums.
Protecting Teeth During Activities: Use mouth guards during sports and avoid using teeth as tools to prevent damage.
Responding to Early Signs: Sensitivity, bleeding gums, or lingering discomfort shouldn’t be ignored. Addressing these concerns early typically leads to simpler treatments.
The Importance of Choosing Local Dental Care
Local practices provide personalized services that larger operations may lack. Families in Cypress appreciate providers who understand their routines and community dynamics, fostering relationships based on trust.
When searching for dental care, many families prioritize local providers. This relationship encourages proactive care and long-term commitments, resulting in fewer last-minute visits.
Patients also benefit from personalized communication. A local practice remembers preferences and follows up with care, establishing a human connection that enhances the overall experience.
Making Informed Orthodontic Choices
Deciding on orthodontic treatment can be daunting, but understanding the process helps set realistic expectations. Reviewing before-and-after pictures offers patients clarity about potential outcomes.
Dentists clarify timelines and daily care requirements, emphasizing the significance of aligned teeth for overall oral health. By prioritizing education over pressure, dental professionals empower families to make informed decisions.
A Long-term Approach to Family Dental Health
Achieving dental wellness requires more than one visit; it necessitates years of thoughtful care and open discussions. Families that embrace this mindset experience fewer emergencies and greater confidence in their dental health.
In Cypress, where community and quality of life are paramount, selecting a dental provider becomes an investment in the family’s future. Family dentistry aims not only to keep teeth healthy but also to promote well-being through preventive care, modern solutions, and effective communication.
Frequently Asked Questions
How often should families visit the dentist?
Typically, every six months, but your dentist may recommend a different schedule based on individual needs.
When should a child first see a dentist?
At age one or when the first tooth appears.
Can adults receive orthodontic treatment?
Absolutely; many adults benefit from braces or clear aligners.
What if a family member is anxious about visiting the dentist?
A patient-centered dental team prioritizes comfort and explains procedures in detail to help ease fears.
What are the benefits of local dental care?
Local practices often offer personalized services, easier follow-ups, and build trust within the community.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom