health
How Sleep Tracking Technology Is Influencing Sleep Health
In recent years, sleep tracking technology has emerged as a pivotal tool in the quest for better sleep health. From wearable devices to sophisticated smartphone applications, these innovations are transforming how we understand and manage our sleep patterns. This article delves into the influence of sleep tracking technology on sleep health, exploring its benefits, limitations, and future potential.
Understanding Sleep Tracking Technology
Sleep tracking technology encompasses a range of devices and applications designed to monitor and analyze sleep patterns. These tools typically measure various parameters such as sleep duration, sleep stages (light, deep, REM), heart rate, breathing patterns, and even movements during sleep. The data collected is then processed to provide insights into the quality and efficiency of one’s sleep.
Wearable devices like fitness trackers and smartwatches are among the most popular sleep tracking tools. These devices are equipped with sensors that can detect physiological signals and translate them into meaningful sleep data. Additionally, there are non-wearable options like under-mattress sensors and bedside monitors that offer similar functionalities without the need for physical contact.
The Benefits of Sleep Tracking Technology
Increased Awareness and Education
One of the most significant benefits of sleep tracking technology is the increased awareness it brings to sleep health. Many individuals are unaware of their sleep habits and the impact of poor sleep on their overall well-being. By providing detailed insights into sleep patterns, these technologies educate users about the importance of sleep and encourage healthier sleep practices.
Personalized Sleep Insights
Sleep tracking technology offers personalized feedback based on individual sleep data. This customization allows users to identify specific issues affecting their sleep, such as frequent awakenings, insufficient REM sleep, or irregular sleep schedules. With this information, individuals can make targeted changes to their habits and environments to improve sleep quality.
Early Detection of Sleep Disorders
Advanced sleep tracking devices can help in the early detection of sleep disorders such as sleep apnea, insomnia, and restless leg syndrome. By monitoring irregularities in breathing, heart rate, and movement, these devices can alert users to potential problems that may require medical attention. Early detection is crucial for timely intervention and treatment.
Behavioral Changes and Habit Formation
The continuous feedback provided by sleep tracking technology can motivate users to adopt healthier sleep habits. For instance, consistent tracking may reveal that late-night screen time negatively impacts sleep quality. Armed with this knowledge, individuals are more likely to make positive behavioral changes, such as reducing screen time before bed or establishing a regular sleep schedule.
Data-Driven Sleep Hygiene
Sleep hygiene refers to the practices and environmental factors that promote good sleep. Sleep tracking technology can help users optimize their sleep environment by identifying factors that disrupt sleep, such as noise, light, or temperature. By making data-driven adjustments, individuals can create a more conducive environment for restful sleep.
Picture by: Yandex.com
Limitations and Challenges
While sleep tracking technology offers numerous benefits, it is not without limitations and challenges.
Accuracy Concerns
The accuracy of sleep tracking devices can vary significantly. Factors such as device quality, sensor placement, and individual differences can affect the reliability of the data. While many devices provide useful approximations, they may not always match the precision of clinical sleep studies conducted in controlled environments.
Over-Reliance on Technology
There is a risk that individuals may become overly reliant on sleep tracking technology, potentially leading to anxiety or obsession over sleep data. This phenomenon, sometimes referred to as “orthosomnia,” can paradoxically result in poorer sleep quality as individuals become fixated on achieving perfect sleep metrics.
Privacy and Data Security
Sleep tracking devices collect sensitive personal data, raising concerns about privacy and data security. Users must be aware of how their data is stored, used, and shared by device manufacturers and application developers. Ensuring robust data protection measures is essential to maintaining user trust.
Cost and Accessibility
High-quality sleep tracking devices can be expensive, limiting accessibility for some individuals. While there are more affordable options available, they may not offer the same level of accuracy or functionality. Bridging this gap is essential to ensure that the benefits of sleep tracking technology are accessible to a broader population.
The Future of Sleep Tracking Technology
The future of sleep tracking technology holds exciting possibilities. Advances in artificial intelligence (AI) and machine learning are poised to enhance the accuracy and predictive capabilities of these devices. AI algorithms can analyze vast amounts of sleep data to identify patterns and correlations that may not be apparent to human observers. This could lead to more precise and personalized sleep recommendations.
Integration with other health monitoring systems is another promising avenue. By combining sleep data with information on physical activity, diet, and mental health, holistic health insights can be derived. This integrated approach can provide a more comprehensive understanding of how various lifestyle factors interact to influence sleep health.
Moreover, the development of non-invasive and contactless sleep tracking technologies is on the horizon. Innovations such as radar-based sensors and advanced imaging techniques can monitor sleep without the need for wearables, offering greater comfort and convenience for users.
Conclusion
Sleep tracking technology is revolutionizing the way we approach sleep health. By providing valuable insights into sleep patterns and promoting awareness, these tools empower individuals to take control of their sleep habits and make informed decisions for better health. However, it is essential to recognize the limitations and challenges associated with these technologies and use them as complementary tools rather than definitive solutions.
As technology continues to evolve, the potential for sleep tracking devices to contribute to our understanding of sleep and overall well-being is immense. By embracing these innovations while maintaining a balanced perspective, we can harness the power of sleep tracking technology to improve sleep health and enhance our quality of life.
Care
Understanding Your Cycle: Benefits of At-Home Ovulation Testing

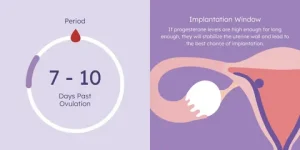
Most women find tracking ovulation tricky due to too many apps, graphs, or clinic visits. Yet knowing when it happens matters whether planning a baby, preventing one, or just being curious about how the body works. A straightforward test you can do at home cuts through the noise. Instead of guessing, there’s now a calm method right on your bathroom counter. That moment each month becomes less mysterious and clearer.
At home, testing means less stress and fewer trips to clinics because tracking happens where life already unfolds. Day by day, results build a picture of what’s normal, simply through routine moments adding up over time.
Easy At-Home Ovulation Test Explained?
A little device used at home can spot when you’re close to ovulating. Because it picks up shifts in natural body chemicals linked to your monthly rhythm. Right before releasing an egg, there’s a rise in a hormone called luteinizing hormone. This spike tells the ovaries it is nearly time to let go of an egg.
A shift in hormones shows up in pee, so tracking helps spot the best time to get pregnant. By checking now and then, cycles make more sense, revealing exactly when chances rise sharply.
Tracking Ovulation Helps Understand Fertility Timing
Ovulation tracking gives women clearer insight into their bodies. Mood shifts, hunger levels, energy, and emotions often tie closely to hormone patterns. When the timing of ovulation is clear, it becomes easier to shape workouts, meals, schedules, and moments for self-care around what feels right.
Finding the right moment when trying to have a baby? Knowing which days are most fertile helps without extra effort. When preventing pregnancy, instead of keeping track of ovulation, backs up non-hormonal choices. Either way around, a simple test you take at home brings clearer answers.
How a Simple At-Home Ovulation Test Works
A shift in hormones shows up in pee just before an egg is released. As those chemicals climb, the strip picks it up with a clear sign. Most of the time, this happens a day or so before ovulation, giving extra time to prepare.
A handful of days ahead of expected ovulation, most women begin checking each morning. As weeks pass, subtle clues emerge, linking together in ways unique to their bodies. Testing becomes routine, day after day, until the shift shows up on the strip.
Easy At-Home Ovulation Test Benefits
What stands out most is how easy it gets. Doing the test inside your place just slips into whatever you already do each morning. There are no scheduled slots to keep, no trips to clinics, and nothing bulky or confusing to set up. Answers show up fast, so there is no pause in your usual flow. The whole thing moves quietly alongside life.
Finding privacy matters a lot to some people. For many women, watching their cycle feels too private for outside eyes. Conducting tests within their own space allows them to progress through each step without drawing attention. Comfort comes easier when no one else is involved.
When things stay routine, it gets simpler. Because the method isn’t complicated, many women tend to check often this builds a clearer picture of their cycle as weeks pass.
Make testing part of daily life
Some women go for a morning check, yet a few pick late hours based on how their day rolls. The key thing? Staying steady. Doing it at the same hour every time brings sharper results into view.
A few cycles in, many notice their ovulation settling into a pattern. Because of this shift, checking each day starts to seem less like work and just part of the flow.
Staying Calm While Reviewing Test Outcomes
First thing you notice might be the mess of numbers. One day blurs into the next, and then suddenly a spike appears. Watch the flow across mornings and evenings rather than fixating on any single mark.
Later on, spotting familiar signs feels more natural. As women discover what their bodies typically do, assurance grows. With that quiet knowing comes less worry and a steadier faith in how tests work.
Things that might change ovulation test outcomes
Tiny shifts happen when life gets busy. Hormone levels react to how you live each day. When stress piles up, everything inside tweaks a bit. Ovulation might move ahead or lag if rest feels scarce. Not drinking enough water plays its part, too. A cold or long trip nudges things off rhythm. The body adjusts without alarm. Tests still work just fine through those small wobbles. Nothing breaks because of ordinary hiccups.
A shift in daily habits can shape how the body behaves, making calm persistence easier for many women. When you watch several monthly cycles unfold, trends begin to stand out, revealing what’s typical for one person.
Feeling at ease with home testing
Finding balance can be tough when trying to conceive, particularly with hormones shifting unpredictably. A straightforward test used privately brings ease, replacing stress with quiet confidence during personal moments.
Out there, away from eyes and clocks, testing becomes something a woman can shape on her own terms. Because of that quiet space, staying with it week after week feels less like effort. Cycle patterns begin to make more sense when seen through a steady, personal rhythm.
People tracking ovulation at home with easy tests?
Starting slow works well for women drawn to minimal effort. Because clarity matters, this approach skips tangled instructions. Those new to monitoring fertility tend to land here first; its rhythm teaches without pressure.
Over time, those tracking each day might start noticing shifts, especially when periods don’t come like clockwork. A different rhythm reveals itself only after several months of watching closely.
Dr. Alan Lindemann, Trusted Fertility & Saliva Ovulation Expert at KNOWHEN
Dr. Alan Lindemann, an experienced obstetrician with nearly four decades of practice and over 6,000 safe deliveries, provides trusted guidance on using the KNOWHEN® saliva ovulation test to track fertile days naturally. He empowers women with expert reproductive health insight, highlighting how this simple, non-invasive, and reusable method makes fertility awareness easier and more confident without clinic visits or complicated procedures. His expert advice supports informed decisions about ovulation timing, cycle understanding, and natural family planning.
In this blog, Dr. Alan shares clear insights on how home ovulation tests help women track fertile days easily and privately. He explains how simple at-home testing detects natural hormonal changes to identify ovulation without clinic visits. Ideal for fertility awareness, cycle understanding, pregnancy planning, or natural birth control, this guide highlights a calm, reliable, and stress-free approach to understanding your body at home.
At-Home Ovulation Tests Compared to Other Approaches
Tracking fertility happens in different ways. Some pick calendars; others check body heat daily instead. Medical tests give data, too. In between watching signs naturally and lab work, there is a middle path. That spot belongs to simple ovulation kits used at home. These tools fit quietly into routines. Information shows up clearly without doctor visits. Not every approach works the same for everyone. Personal rhythm matters most when trying to understand timing.
Fresh data on hormones shows up instantly; no doctor trips needed. Some pair those results with notes on their monthly patterns along with physical cues, building clearer pictures of when they might conceive.
Tracking Ovulation Changes Across Time
Month by month, watching for ovulation gives women clearer insight into how their cycle works. Suddenly, shifts in energy levels, emotions, or body signals feel less confusing. With that clarity comes a stronger sense of balance and more space to listen to what the body needs.
Each day of checking brings you closer to how your body works. Slowly, knowing about fertility fits into daily life without pressure.
Conclusion
Home ovulation tests make spotting fertile times straightforward, minus the stress. Hormone shifts give clear signs when checked each day privately. Comfort grows from routine testing, away from clinics or judgment. Personal timing becomes clearer through steady observation, nothing more.
A clearer understanding of fertility often develops slowly, through consistent effort over time. Ovulation can make sense without confusion or stress. Small routines each day might reveal what matters most.
FAQs
Can an easy at-home ovulation test be used with irregular cycles?
Frequently, spotting trends takes longer when periods are unpredictable. Yet sticking with regular checks usually shows useful clues eventually.
Is it normal to see different results each month?
Of course. Body chemistry adjusts on its own when daily habits shift, stress piles up, rest drops off, or wellness dips, throwing cycle cues out of sync.
Business
Revenue Cycle with Expert Medical Coding and RCM Solutions

In the ever-evolving landscape of healthcare, ensuring streamlined revenue flow is crucial for providers. Our medical coding and revenue cycle management (RCM) solutions are meticulously designed to intertwine accurate medical coding with comprehensive financial processes. By aligning clinical documentation, coding precision, and billing workflows, we empower healthcare organizations to minimize claim errors, bolster compliance, and achieve faster reimbursements.
Understanding Medical Coding and RCM Solutions
Medical coding and RCM solutions are not just technical necessities; they are foundational elements that govern the financial lifecycle of healthcare services. This holistic approach encompasses:
- Clinical Documentation Review: Ensuring that every detail is accurately captured.
- ICD-10, CPT, and HCPCS Coding: Assigning codes that reflect diagnoses and procedures.
- Charge Capture and Validation: Confirming all billable services are accounted for.
- Claim Submission and Tracking: Sending claims systematically for timely processing.
- Denial Management and Appeals: Addressing and correcting rejected claims.
- Payment Posting and Reconciliation: Ensuring accurate recording of payments received.
By integrating these elements, we establish a streamlined workflow where coding accuracy directly enhances reimbursement efficiency.

Comprehensive Medical Coding Services
At the heart of our offering is a commitment to high-quality, accurate medical coding:
Accurate Medical Coding Services
Our team of certified coders ensures compliance with the latest coding standards, including:
- ICD-10-CM for diagnoses
- CPT for procedures
- HCPCS Level II for supplies and non-physician services
Charge Capture and Validation
We ensure that every eligible service is accurately captured and validated to prevent undercoding and missed revenue opportunities.
Claim Submission and Management
We prioritize clean claim submissions and maintain continuous tracking to guarantee timely responses from payers.
Denial Management and Appeals
Identifying patterns in denials enables us to rectify coding errors and file appeals, contributing to revenue recovery.
Payment Posting and A/R Follow-ups
By ensuring accurate payment posting and proactive accounts receivable management, we enhance cash flow and reduce outstanding balances.
The Importance of Medical Coding Accuracy
Accurate coding forms the backbone of an effective revenue cycle. Errors in coding can lead to several detrimental outcomes, including:
- Claim Denials and Rejections: Errors result in lost revenue and wasted resources.
- Delayed Reimbursements: Inaccuracies can hinder timely payments from insurers.
- Compliance and Audit Risks: Mistakes may lead to severe legal repercussions.
- Revenue Loss: The cumulative effect of errors can significantly impact a healthcare provider’s bottom line.
Our solutions ensure that accuracy is maintained at every step, safeguarding both revenue and compliance.
Benefits of Outsourcing Medical Coding and RCM Solutions
Opting to outsource your coding and RCM processes can provide numerous advantages:
- Access to Certified Professionals: Our team comprises seasoned coding experts, certified in their fields.
- Reduced Administrative Burdens: Outsourcing alleviates the workload, allowing staff to focus on patient care.
- Improved Claim Acceptance Rates: Our expertise results in fewer claim rejections.
- Faster Reimbursements: Efficient management accelerates payment cycles.
- Cost-Effectiveness: Outsourcing reduces operational costs significantly without compromising quality.
- Regulatory Compliance: We ensure alignment with CMS guidelines and payer requirements.
This shift allows healthcare providers to dedicate more time to the core mission of patient care, minimizing administrative distractions.
Our Streamlined Workflow
Our RCM workflow is designed to optimize every facet of the revenue cycle:
- Clinical Documentation Review: Ensure completeness and correctness.
- Accurate Code Assignment: Use the right codes to reflect services accurately.
- Charge Capture Validation: Confirm billable services before submission.
- Clean Claim Submission: Submit claims in a timely manner.
- Payment Posting and Reconciliation: Record payments accurately to protect revenue.
- Denial Analysis and Appeals: Correct errors and address denials proactively.
- Continuous Performance Monitoring: Regular check-ins to assess workflow efficiency.
Each of these steps is crafted to maximize revenue and minimize errors.
Who Can Benefit from Medical Coding and RCM Solutions?
Our comprehensive solutions are beneficial for a variety of healthcare entities, including:
- Hospitals and Health Systems
- Physician Practices
- Urgent Care Centers
- Specialty Clinics
- Behavioral Health Providers
- Medical Billing and RCM Companies
Large or small, our scalable solutions can adapt to each organization’s unique operational needs.
Why Choose ASP RCM Solutions?
Here’s why our clients trust us with their RCM needs:
- Expertise: Our team consists of certified medical coders with vast experience across multiple specialties.
- End-to-End RCM Services: We offer comprehensive solutions tailored to your needs.
- Compliance Assurance: Our workflows are designed to meet HIPAA standards, ensuring confidentiality.
- Proven Results: We have decreased denials and improved accounts receivable days.
- Transparent Reporting: Clients receive regular updates on their financial performance.
Our mission is to deliver accuracy, compliance, and sustainable revenue growth.
Frequently Asked Questions (FAQs)
What are medical coding RCM solutions?
These solutions integrate accurate coding with revenue cycle management to ensure efficient billing and expedient reimbursements.
How do coding errors affect RCM?
Errors can lead to claim denials, delayed payments, and compliance concerns, ultimately affecting revenue performance.
Do you support ICD-10, CPT, and HCPCS coding?
Absolutely! Our services encompass full coding support across all standard systems.
Can outsourcing improve cash flow?
Indeed, accurate coding and proactive RCM practices significantly enhance reimbursement timeliness and consistency.
Are your services compliant with applicable regulations?
Yes, we adhere to CMS guidelines, payer requirements, and HIPAA regulations.
Get Started with Our Medical Coding RCM Solutions
Partner with us for reliable medical coding and RCM solutions that ensure accuracy, compliance, and optimized financial performance. Optimize your revenue cycle and enhance reimbursements with assurance. Our tailored RCM solutions serve hospitals, clinics, and practices of every scale.
Patient Eligibility and Insurance Verification
Effective verification helps avoid claim rejections and clarifies financial responsibilities for patients.
Comprehensive Medical Coding and Charge Capture
Our certified coders guarantee precise coding to minimize errors and compliance issues.
Efficient Claim Submission and Management
Claims are submitted efficiently and tracked continuously for quicker responses from payers.
Accurate Payment Posting
We ensure correct payment postings and resolve discrepancies proactively to safeguard your revenue.
Denial Management and Appeals
Our experienced team analyzes denial trends and promptly submits appeals to recover missed revenue.
Accounts Receivable Follow-ups
Proactive follow-ups on A/R reduce outstanding balances and enhance cash flow.
Why Medical RCM Solutions Are Essential
In the absence of effective RCM, healthcare providers risk facing increased claim denials, delays in reimbursements, revenue leakage, compliance risks, and operational inefficiencies. Our medical RCM solutions address these challenges, creating a transparent and compliant billing workflow.
Final Thoughts
Outsourcing your RCM processes can transform your healthcare practice by reducing administrative burdens and enhancing revenue cycle efficiency. Experience financial stability and long-term growth by partnering with us for your medical coding and RCM needs. Let us help you streamline your revenue cycle and maximize your reimbursements effectively.
Consumer Services
Gift of Health This Valentine’s Day: GTA Fitness Gym Equipment

Valentine’s Day is traditionally associated with flowers, chocolates, and romantic gestures—but this year, why not give a gift that truly makes a lasting impact? Instead of a fleeting present, consider investing in the health and fitness of your loved ones. GTA Fitness, a leading provider of premium fitness equipment in Canada, is offering an exclusive Valentine’s Day Gym Equipment Sale. From essential home gym accessories to full workout setups, it’s the perfect opportunity to show care while promoting long-term wellness.
Why Fitness Equipment Makes the Perfect Valentine’s Day Gift
Gifting fitness equipment is thoughtful, practical, and impactful. Unlike consumable gifts that are quickly used or forgotten, gym equipment provides years of value. Choosing a gift that encourages exercise shows that you care about your loved one’s health, wellbeing, and lifestyle. Key benefits include:
-
Promotes Health and Longevity: Encourages consistent exercise for heart, joint, and muscle health
-
Builds Strength and Mobility: Helps improve overall fitness and reduce the risk of injuries
-
Motivation and Accountability: Having equipment at home makes workouts more accessible and consistent
-
Fun and Engagement: Couples or friends can workout together, making fitness a social and enjoyable activity
Whether your partner is a beginner, a fitness enthusiast, or someone who wants to start their journey, GTA Fitness offers a wide range of equipment that can meet all needs.

Top Gym Equipment to Consider for Valentine’s Day
-
Dumbbells and Weight Sets
Dumbbells are versatile, portable, and essential for full-body strength training. They allow for exercises like squats, lunges, presses, and rows, targeting multiple muscle groups. GTA Fitness offers premium dumbbell sets with adjustable weights to cater to both beginners and advanced lifters. Gifting a dumbbell set ensures your loved ones can perform a variety of workouts from the comfort of home. -
Workout Benches
Benches are a key component for many exercises such as bench presses, chest flys, step-ups, and seated presses. Adjustable benches provide additional versatility, allowing for flat, incline, and decline positions. GTA Fitness benches are ergonomically designed with durable frames and thick padding for comfort and safety. They serve as the foundation of a home gym, helping users target multiple muscle groups efficiently. -
Resistance Bands
Resistance bands are lightweight, portable, and extremely versatile. They help tone muscles, increase strength, and improve flexibility. From glute bridges and squats to arm exercises and stretching routines, resistance bands can be incorporated into countless workouts. GTA Fitness offers bands in various resistance levels, allowing for progressive training that adapts to the user’s strength and fitness level. -
Cardio Machines
Cardio machines like treadmills, ellipticals, and stationary bikes are excellent for cardiovascular health, endurance, and calorie burning. A treadmill allows for walking, jogging, or running indoors regardless of weather, while an elliptical provides a low-impact, full-body cardio experience. GTA Fitness cardio equipment is built for smooth operation, durability, and comfort, making it perfect for daily use at home or in professional setups. -
Full Home Gym Sets
For serious fitness enthusiasts, a complete home gym setup is the ultimate gift. These multi-functional machines allow a variety of exercises including presses, pulls, curls, and leg workouts—all in one compact design. GTA Fitness home gym systems combine strength training, cardio, and flexibility tools, creating a comprehensive solution for any fitness goal. These setups are ideal for couples who want to train together or anyone looking for a premium fitness solution.
Benefits of Gifting Gym Equipment
-
Encourages Consistent Workouts: Having equipment at home reduces excuses and promotes regular exercise
-
Supports Strength and Confidence: Strength training boosts self-esteem while improving overall body composition
-
Long-Term Value: Unlike short-lived gifts, gym equipment provides ongoing benefits for years
-
Promotes Shared Experiences: Couples or friends can workout together, making fitness fun and motivating
-
Adaptable for Any Fitness Level: Whether beginner or advanced, there’s equipment suitable for everyone
Tips for Choosing the Right Gym Equipment
-
Understand Their Fitness Goals: Determine whether your loved one is focused on strength, cardio, flexibility, or full-body training.
-
Measure Available Space: Ensure the equipment fits comfortably in their home or workout area.
-
Choose High-Quality Equipment: GTA Fitness products are durable, safe, and built to last.
-
Consider Usability: Select equipment that matches the user’s experience level, especially for beginners.
-
Balance Cost and Value: GTA Fitness offers a wide range of options that suit different budgets without compromising quality.
GTA Fitness Valentine’s Day Sale Highlights
-
Special offers on dumbbells, benches, resistance bands, and complete home gym configurations
-
Special offers on cardio machines suitable for couples and fitness enthusiasts
-
High-quality, durable, and safe equipment designed to last for years
-
Expert guidance and customer support to help select the right products
-
Flexible options for home gyms, small spaces, or professional setups
Tips to Make Your Fitness Gift Extra Special
-
Include a personalized workout plan or fitness challenge for motivation
-
Pair equipment with accessories like yoga mats, water bottles, or gloves
-
Write a motivational note or provide a fitness journal to track progress
-
Offer to join workouts together to make fitness a shared, fun experience
-
Create a themed gift package: combine resistance bands, dumbbells, and a workout guide for a thoughtful present
Why Fitness Gifts Make a Difference
Unlike traditional gifts, fitness equipment is meaningful and practical. It shows you care about your loved one’s health, goals, and long-term wellbeing. It also encourages habits that improve overall physical and mental health. Giving the gift of fitness this Valentine’s Day means investing in something that benefits your loved ones daily—far beyond a single occasion.
Conclusion
This Valentine’s Day, step away from ordinary gifts and give something that truly matters: the gift of health, strength, and motivation. GTA Fitness’ Valentine’s Day Gym Equipment Sale offers a wide range of high-quality products for all fitness levels. From dumbbells and benches to full home gym systems, these gifts empower your loved ones to stay active, strong, and inspired. Celebrate love in a meaningful way by supporting their fitness journey—because showing you care about their health is the ultimate expression of love.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom




































