health
Legal Battles Emerge Over AI in Health Insurance Claims Processing

Introduction
In a rapidly evolving landscape where technology intersects with healthcare, lawsuits are emerging as a focal point, challenging the use of artificial intelligence (AI) tools by health insurance companies in the processing of claims. These legal challenges not only raise questions about the legality and fairness of such practices but also have profound implications for both insurers and policyholders. To shed light on the legal intricacies and potential shifts in the use of AI in healthcare, we turn to Dr. Emily Juris Insight, AI-driven insurance processes a legal analyst specializing in healthcare and technology law.
The Legal Landscape: Lawsuits Unveiled

This image is taken from google.com
Recent lawsuits have brought attention to the deployment of AI tools by health insurance companies for claims processing. The key legal concerns include:
- Transparency and Accountability:
- Issue: Lack of transparency in how AI algorithms process and evaluate claims.
- Implication: Challenges in holding companies accountable for claim denials or delays attributed to AI decisions.
- Algorithmic Bias and Fairness:
- Issue: Allegations of algorithmic bias leading to disparate treatment of certain policyholders.
- Implication: Potential violations of anti-discrimination laws and AI-driven insurance processes ethical concerns related to fairness in claims processing.
- Informed Consent:
- Issue: Policyholders often unaware of the use and impact of AI in claims processing.
- Implication: Legal questions surrounding the need for informed consent and disclosure of AI involvement in decision-making.
Comparative Table: Legal Concerns in AI-Driven Claims Processing
| Legal Concerns | Before Lawsuits | Amid Emerging Lawsuits |
|---|---|---|
| Transparency and Accountability | Limited clarity on AI decision-making processes. | Increased scrutiny on transparency and accountability, demanding clearer insights into AI-driven claims processing. |
| Algorithmic Bias and Fairness | Concerns about potential bias but limited legal challenges. | Allegations of bias leading to legal scrutiny and potential violations of anti-discrimination laws. |
| Informed Consent | Limited awareness among policyholders about AI involvement. | Legal questions arise about the necessity for informed consent and disclosure of AI use in claims processing. |
Implications for Health Insurance Companies

This image is taken from google.com
- Reassessment of AI Deployment:
- Consideration: Health insurance companies may need to reassess the ethical and legal implications of AI tools.
- Implication: Potential adjustments in the deployment and communication of AI technologies in claims processing.
- Legal Compliance and Risk Mitigation:
- Consideration: Enhanced efforts to ensure compliance with existing laws and mitigate legal risks.
- Implication: A proactive approach to address legal concerns and AI-driven insurance processes prevent potential litigation.
- Ethical AI Frameworks:
- Consideration: Development and adherence to ethical AI frameworks.
- Implication: Building public trust and minimizing legal challenges through the adoption of ethical guidelines in AI use.
Comparative Table: Implications for Health Insurance Companies
| Implications | Before Lawsuits | Amid Emerging Lawsuits |
|---|---|---|
| Reassessment of AI Deployment | Limited legal scrutiny and ethical considerations. | Potential adjustments in the deployment and communication of AI technologies in response to legal challenges. |
| Legal Compliance and Risk Mitigation | General efforts to comply with existing laws. | Proactive measures to ensure compliance and mitigate legal risks associated with AI use in claims processing. |
| Ethical AI Frameworks | Varied approaches to ethical considerations. | Increased emphasis on adopting and adhering to ethical AI frameworks to build public trust and address legal concerns. |
Considerations for Policyholders

This image is taken from google.com
- Understanding AI Involvement:
- Recommendation: Policyholders should seek clarity on the role of AI in claims processing.
- Implication: Informed policyholders can better understand the decision-making processes and potential implications for their claims.
- Advocacy for Transparency:
- Recommendation: Advocacy for increased transparency in AI-driven decision-making.
- Implication: Collective efforts may drive changes in industry practices, ensuring fair and transparent claims processing.
- Legal Rights Awareness:
- Recommendation: Awareness of legal rights in the context of AI-driven decisions.
- Implication: Empowered policyholders may take informed action in case of claim denials or delays attributed to AI.
Comparative Table: Considerations for Policyholders
| Considerations | Before Lawsuits | Amid Emerging Lawsuits |
|---|---|---|
| Understanding AI Involvement | Limited awareness of AI’s role in claims processing. | Increasing importance for policyholders to seek clarity on AI involvement and its potential impact on claims. |
| Advocacy for Transparency | Limited collective efforts to advocate for transparency. | Growing advocacy for increased transparency in AI-driven decision-making, potentially driving industry changes. |
| Legal Rights Awareness | Varied levels of awareness about legal rights related to AI decisions. | Increasing awareness among policyholders about their legal rights in the context of AI-driven decisions. |
Future of AI in Healthcare Claims Processing
As the legal landscape evolves, Dr. Emily Juris Insight anticipates a transformative period for AI in healthcare claims processing. Future considerations may include:
- Regulatory Frameworks:
- Prediction: Potential development of regulatory frameworks specifically addressing AI use in healthcare claims processing.
- Implication: Clearer guidelines for companies and increased legal protections for policyholders.
- Ethical Standards:
- Prediction: Heightened emphasis on ethical standards in AI deployment.
- Implication: Industry-wide adoption of ethical guidelines to ensure fairness and prevent legal challenges.
- Public Dialogue:
- Prediction: Increased public dialogue and awareness about AI in healthcare.
- Implication: Informed discussions shaping the future of AI use in healthcare, with a focus on transparency and accountability.
Comparative Table: Future Considerations for AI in Healthcare Claims Processing
| Considerations | Before Lawsuits | Amid Emerging Lawsuits |
|---|---|---|
| Regulatory Frameworks | Limited specific regulations addressing AI in healthcare claims. | Potential development of regulatory frameworks providing clearer guidelines for AI use in claims processing. |
| Ethical Standards | Varied industry approaches to ethical considerations. | Heightened emphasis on adopting ethical standards in AI deployment to ensure fairness and prevent legal challenges. |
| Public Dialogue | Limited public awareness and dialogue about AI in healthcare claims processing. | Increased public dialogue and awareness, shaping the future of AI use in healthcare with a focus on transparency and accountability. |
Conclusion:
Lawsuits challenging the use of AI tools by health insurance companies in claims processing highlight the evolving legal landscape in healthcare. Dr. Emily Juris Insight’s analysis and the provided tables offer insights into the legal concerns, implications for insurers and policyholders, and potential future shifts in the use of AI in healthcare claims processing. As the industry navigates these legal challenges, transparency, ethical considerations, and public dialogue are poised to play crucial roles in shaping the future of AI in healthcare.
health
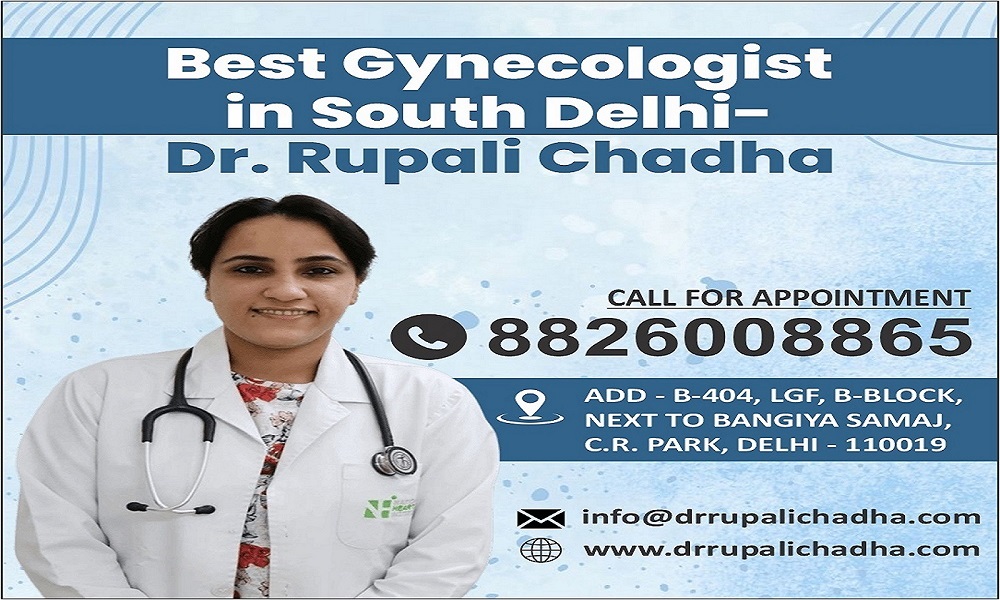
Leading Women’s Health Expert: Best Gynecologist Doctor in Delhi
Introduction
When it comes to women’s health, finding the Best Gynecologist Doctor in Delhi isn’t just about credentials it’s about trust, compassion, and expertise. Delhi, being home to some of India’s top healthcare professionals, has one name that shines brightly in women’s wellness Dr. Rupali Chadha.
She’s more than just a doctor; she’s a guiding light for women seeking holistic, personalized, and advanced gynecological care. Whether it’s regular checkups, maternity support, or managing complex conditions like PCOS, Dr. Chadha’s dedication sets her apart.
Understanding Women’s Health Needs
Women’s health is multifaceted it’s not just about reproduction but also hormonal balance, mental well-being, and preventive care. From adolescence to menopause, every stage requires unique medical attention. Having a reliable gynecologist ensures that women receive consistent care throughout life’s transitions.
Why Choosing the Right Gynecologist Matters?
Choosing the Best Gynecologist Doctor in Delhi can make a world of difference in how a woman experiences healthcare. The right doctor listens, explains, and treats not just the symptoms but the root causes. Women need a safe space to discuss intimate issues, and that’s exactly what Dr. Rupali Chadha provides empathy mixed with clinical excellence.
Meet Dr. Rupali Chadha: The Best Gynecologist Doctor in Delhi
Dr. Rupali Chadha is widely regarded as the Best Gynecologist Doctor in Delhi, known for her blend of medical precision and compassionate care. With years of experience in obstetrics, gynecology, and women’s reproductive health, she’s transformed countless lives.
Her commitment goes beyond treatment she focuses on education, empowerment, and long-term wellness for every patient she meets.
Educational Background and Expertise
Dr. Chadha’s medical journey is rooted in deep academic excellence. Trained at leading institutions and continuously updating her knowledge, she’s equipped with both clinical skills and modern medical insights. Her areas of expertise include:
- High-risk pregnancy management
- Infertility and reproductive health
- Menstrual irregularities
- PCOS and hormonal disorders
- Menopause and post-menopausal care
It’s this combination of experience and empathy that truly defines her as the Best Gynecologist Doctor in Delhi.
Comprehensive Women’s Health Services Offered
Dr. Rupali Chadha offers an extensive range of gynecological services, ensuring every woman finds the support she needs.
1. Routine Check-Ups and Preventive Screenings
Regular checkups are key to maintaining reproductive health. Dr. Chadha focuses on preventive screenings for cervical cancer, breast examinations, and reproductive tract infections — ensuring early detection and treatment.
2. Pregnancy and Maternity Care
For expecting mothers, finding the Best Gynecologist Doctor in Delhi is crucial. Dr. Chadha offers end-to-end maternity care — from prenatal counseling to postnatal recovery — ensuring a healthy journey for both mother and baby.
3. Menstrual Disorders Management
Irregular periods, excessive pain, or abnormal bleeding — Dr. Chadha helps identify underlying causes and tailors treatments to bring hormonal balance and comfort.
4. PCOS and Hormonal Imbalance Treatment
Polycystic Ovary Syndrome (PCOS) affects millions of women, and timely treatment is vital. Dr. Rupali Chadha, known as the Best PCOS Doctor Near Me, provides a holistic approach combining lifestyle guidance, medication, and counseling to restore balance naturally.
Best PCOS Doctor Near Me: Why Dr. Rupali Chadha Stands Out?
Finding a trustworthy PCOS Doctor Near Me can be overwhelming, but Dr. Chadha simplifies this with her patient-first approach. She doesn’t just prescribe medication she understands your lifestyle, stress levels, and emotional well-being. Her customized plans focus on long-term relief, fertility improvement, and overall hormonal harmony.
1. Advanced Facilities and Modern Technology
As the Best Gynecologist Doctor in Delhi, Dr. Chadha’s clinic is equipped with cutting-edge technology for diagnosis and treatment. From 3D ultrasounds to advanced fertility evaluations, she ensures every patient benefits from precision-driven care.
2. Patient-Centric Approach to Women’s Wellness
What truly makes Dr. Chadha special is her human touch. She listens patiently, explains every procedure in simple terms, and never rushes appointments. Women feel heard, respected, and cared for qualities that define the Best Gynecologist in South Delhi.
3. Personalized Treatment Plans for Every Woman
No two women are the same and Dr. Rupali Chadha knows it well. She designs personalized care plans that consider a woman’s age, health background, and lifestyle. Whether you’re seeking fertility assistance, PCOS management, or general wellness, her tailored approach ensures lasting results.
4. Testimonials and Success Stories
Many patients describe Dr. Chadha as a “life-changer.” From resolving years of menstrual pain to helping couples achieve their dream of parenthood, her success stories speak volumes. This unwavering trust is what makes her the Best Gynecologist Doctor in Delhi.
Why Dr. Rupali Chadha is Recognized as the Best Gynecologist Doctor in Delhi?
Her unmatched expertise, state-of-the-art clinic, and heartfelt compassion make her the go-to doctor for thousands of women. Dr. Chadha’s commitment to women’s health has earned her numerous accolades and a loyal patient community across Delhi.
1. Tips for Women to Maintain Reproductive Health
- Schedule regular gynecological checkups.
- Maintain a balanced diet rich in iron and vitamins.
- Exercise regularly to keep hormones balanced.
- Avoid stress it plays a huge role in hormonal health.
- Never ignore irregularities like missed periods or pelvic pain.
2. When to Visit a Gynecologist: Don’t Ignore These Signs?
If you’re experiencing any of the following, it’s time to visit the Best Gynecologist Doctor in Delhi:
- Irregular menstrual cycles
- Persistent abdominal pain
- Difficulty in conceiving
- Unusual discharge or odor
- Sudden weight changes due to hormonal imbalance
Conclusion
Women’s health deserves dedicated care, and Dr. Rupali Chadha ensures exactly that. Her reputation as the Best Gynecologist Doctor in Delhi comes from years of experience, trust, and patient satisfaction. Whether you’re seeking a PCOS Doctor Near Me, fertility help, or general reproductive guidance Dr. Chadha’s expertise can make a life-changing difference.
health
Sour Watermelon Gummies THC: Sweet, Tangy Way to Enjoy Cannabis

Introduction
If you enjoy cannabis but want a tasty, easy-to-use option, Sour Watermelon Gummies with THC might be just what you need. These gummies combine the sharp, tangy flavor of sour watermelon with the relaxing and enjoyable effects of THC. Edible cannabis products like these gummies are becoming popular because they offer a fun and discreet way to consume THC without smoking or vaping. In this article, we will explore what Sour Watermelon Gummies THC are, their benefits, how they work, and tips for safe use.
What Are Sour Watermelon Gummies THC?
Sour Watermelon Gummies THC are chewy, fruit-flavored candies infused with tetrahydrocannabinol (THC), the main psychoactive compound in cannabis. These gummies deliver a controlled dose of THC in each piece, making it easier for users to manage their intake. The sour watermelon taste adds a delicious twist, combining sweetness with a tangy kick that many people love.
How Do THC Gummies Work?
When you eat a THC gummy, your body processes it differently than when you smoke or vape cannabis. The THC is absorbed through the digestive system, and it takes longer to feel the effects—usually between 30 minutes to 2 hours. However, the effects also last longer, often 4 to 8 hours. This makes gummies a good choice for people who want long-lasting relief or enjoyment without the smell or harshness of smoke.
Benefits of Sour Watermelon Gummies THC
There are many benefits to choosing Sour Watermelon Gummies THC. First, they offer a tasty and simple way to consume cannabis without harsh smoke or strong smells. The flavor is fun and refreshing, making it easier for some people to enjoy cannabis. Gummies also provide a consistent dose of THC, which helps users control how much they take. This can make the experience safer and more comfortable. Because they are small and easy to carry, gummies are a convenient option for those who want cannabis on the go or want to avoid smoking in public.
There are several reasons why people choose sour watermelon THC gummies:
- Discreet and Convenient: Gummies look like regular candy, so you can enjoy them anywhere without drawing attention.
- Precise Dosage: Each gummy contains a set amount of THC, helping you control how much you consume.
- No Smoking Required: This option is great for those who dislike smoking or have breathing issues.
- Long-Lasting Effects: Because gummies are digested slowly, their effects last longer compared to other cannabis forms.
- Delicious Flavor: The sour watermelon taste makes taking cannabis enjoyable and fun.
Role of Sour Watermelon Gummies THC

Image by: Yandex.com
Sour Watermelon Gummies THC play an important role in making cannabis more accessible and enjoyable. They offer a way for people to experience cannabis without using traditional methods like smoking. This can attract new users who might be nervous about trying cannabis. Gummies also provide a clear, measured dose, which helps users better understand how cannabis affects them. This role is important for safe and responsible use. Additionally, flavored gummies add variety to the cannabis market, offering something fun and tasty compared to other products.
Who Should Use Sour Watermelon Gummies THC?
These gummies are popular among both recreational users and those who use cannabis for medical reasons. People dealing with pain, anxiety, or insomnia often find gummies helpful because of the steady, long-lasting relief they provide. However, beginners should start with a small dose and wait before taking more to avoid unpleasant effects.
How to Use Sour Watermelon Gummies THC Safely
If you’re new to THC gummies or edibles, it’s important to follow some simple safety tips:
- Start Low, Go Slow: Begin with a low dose, like 5 mg of THC or less, and wait at least two hours before taking more.
- Read Labels: Always check the product packaging for THC content and any other ingredients.
- Store Properly: Keep gummies out of reach of children and pets since they look like regular candy.
- Avoid Mixing: Don’t mix THC gummies with alcohol or other drugs, as this can increase side effects.
- Know the Laws: Make sure cannabis edibles are legal in your area before buying or using them.
Possible Side Effects of THC Gummies
While many people enjoy THC gummies safely, some may experience side effects such as dry mouth, dizziness, or increased heart rate. In rare cases, high doses can cause anxiety or paranoia. If you feel uncomfortable, it’s best to relax in a safe place and stay hydrated. If symptoms persist, seek medical advice.
How to Choose Quality Sour Watermelon Gummies THC
Not all THC gummies are created equal. To find the best product, look for:
- Lab Testing: Choose gummies tested by third-party labs to ensure quality, potency, and safety.
- Clear Labeling: The package should clearly state THC dosage, ingredients, and warnings.
- Reputable Brands: Buy from trusted manufacturers or dispensaries with good customer reviews.
- Natural Ingredients: Avoid gummies with artificial colors or harmful additives.
Where to Buy Sour Watermelon Gummies THC
In places where cannabis is legal, you can find these gummies at licensed dispensaries or online stores. Always buy from authorized sellers to avoid fake or unsafe products. If you live in an area where cannabis is not legal, it is important to follow local laws and avoid unregulated sources.
Conclusion
Sour Watermelon Gummies THC offer a tasty, discreet, and effective way to enjoy the benefits of cannabis. With their sweet and tangy flavor, precise dosing, and long-lasting effects, these gummies are a popular choice for many users. Whether you want relief from pain or just a fun way to relax, sour watermelon THC gummies can be a great option. Remember to start with a low dose, use them responsibly, and always choose high-quality products from trusted sources. This way, you can enjoy the sweet and sour experience safely and confidently.
health
MedBillionaires: Transforming Healthcare Through AI and FinTech

Introduction
In a world where healthcare and finance are closely linked, MedBillionaires™ leads the way in innovation, connecting medical technology with financial intelligence. As a Pre-Public Company™ (PPC™), MedBillionaires™ is changing how MedTech companies are built and scaled, offering a model that has the governance and structure of a public company, but without being listed.
The company’s goal is to create a large, AI-driven Med-FinTech ecosystem that connects every part of the medical supply chain, from production to patient care. This smart system improves efficiency, transparency, and cost-effectiveness, making MedBillionaires™ a game-changer in healthcare technology.
What is MedBillionaires?
MedBillionaires is an innovative platform that combines AI and FinTech to improve both healthcare services and financial solutions for people and organizations. Using advanced technology, MedBillionaires aims to cut costs, improve patient care, and make healthcare finances more efficient.
What makes MedBillionaires special is its mix of medical knowledge and tech innovation. With AI-driven tools, they predict medical needs, offer personalized health plans, and help manage healthcare costs.
At its heart, MedBillionaires is focused on making healthcare smarter, more efficient, and more affordable, while also simplifying financial processes that are usually complicated and unclear.
How AI is Transforming Healthcare at MedBillionaires
Artificial Intelligence (AI) has become one of the most influential technologies in modern healthcare. Its capabilities range from enhancing patient diagnosis to streamlining treatment plans and improving administrative efficiency. MedBillionaires leverages AI in several key ways to transform the healthcare experience:
1. Predictive Analytics for Better Care
AI’s ability to analyze large datasets allows MedBillionaires to offer predictive analytics that can anticipate patient needs. By processing vast amounts of health data, AI can detect patterns and provide insights into potential health risks, enabling early interventions and personalized care. For example, AI algorithms can analyze a patient’s medical history, lifestyle, and genetic information to suggest preventive measures or treatments, minimizing the risk of serious health issues in the future.
2. Improved Diagnostics
AI is helping doctors diagnose conditions faster and with greater accuracy. By integrating AI into diagnostic tools, MedBillionaires makes it easier for healthcare professionals to analyze medical images, lab results, and other diagnostic data. For instance, AI can detect anomalies in radiology scans that might be overlooked by the human eye, providing doctors with valuable second opinions that improve diagnostic accuracy.
3. Remote Monitoring and Telemedicine
With the growing trend of telemedicine, AI plays a critical role in monitoring patients remotely. MedBillionaires has incorporated AI-driven devices that track vital signs, such as heart rate, blood pressure, and glucose levels, allowing healthcare providers to monitor patients without needing them to visit a hospital. AI-powered telemedicine platforms also enable doctors to offer consultations and treatment advice remotely, reducing the need for in-person visits and increasing the accessibility of healthcare services.
4. Personalized Treatment Plans
MedBillionaires utilizes AI to craft personalized treatment plans based on the unique needs of each patient. By considering a range of factors—medical history, lifestyle, genetic predisposition—AI can help design customized plans that increase the likelihood of successful outcomes. Whether it’s medication recommendations, lifestyle changes, or therapy sessions, AI ensures that patients receive tailored treatments that align with their specific conditions.
The Pre-Public Company™ Model
Unlike regular startups, MedBillionaires™ builds private companies to work like publicly traded ones right from the start. This structure helps businesses grow sustainably, attract investors, and stay accountable.
By adding strong governance, transparency, and performance standards early on, MedBillionaires™ sets businesses up for long-term success. The PPC™ model removes common challenges when scaling, making sure every company is “ready for the public” from day one. It’s an innovative approach that blends new ideas with business maturity, changing how MedTech companies grow.
Building the Med-FinTech Ecosystem
At the heart of MedBillionaires™ is a digital platform powered by Artificial Intelligence, designed to improve healthcare financing, logistics, and data management. The platform connects healthcare providers, medical manufacturers, distributors, and financial institutions into one smart system.
Using AI and data analytics, the company makes every part of the medical supply chain more efficient, increasing productivity. This mix of MedTech and FinTech creates a smooth environment where innovation and accessibility come together. Examples include financial automation, secure digital payments, and credit systems for medical suppliers, all of which are changing traditional healthcare business models.
AI: The Core of the Future
Artificial Intelligence is the heart of MedBillionaires™. The company uses AI not just for automation, but to make smart decisions. From AI-powered diagnostics to predicting trends in healthcare financing, MedBillionaires™ integrates machine learning into everything it does.
AI helps improve medical accuracy, predict supply chain issues, and optimize resource use. For hospitals, startups, and investors, this means better insights, lower costs, and better patient outcomes. MedBillionaires™ believes the future of healthcare is all about AI-driven, financially smart systems.
Global Vision, Local Impact
MedBillionaires™ operates globally but also makes a local impact by supporting healthcare innovation in emerging markets. Its business model helps small and mid-sized MedTech companies grow in a sustainable way.
In places like Lahore and Gulberg, where healthcare startups are growing fast, MedBillionaires™ provides a platform for local companies to expand globally. By combining AI, finance, and strong governance, it helps Pakistani MedTech startups compete internationally while staying true to their local roots.
Working with medical innovators and tech companies helps build smarter, data-driven healthcare systems. This mix of AI and Med-FinTech creates a connected ecosystem that benefits both patients and businesses.
The Importance of Digital Presence
In today’s digital era, visibility and communication are crucial. MedBillionaires™ understands this and emphasizes building a strong digital footprint through Instagram, Facebook, and professional networks. These platforms enhance engagement, share thought leadership, and connect investors and innovators.
To explore MedBillionaires™’ ecosystem in more detail, visit their official page (internal link) to learn how AI and FinTech are shaping the future of healthcare.
Collaboration and Industry Influence
Partnerships are key to helping MedBillionaires™ grow. The company works with top MedTech companies, research groups, and financial innovators to strengthen its AI platform.
Forbes Health and HealthTech Magazine say that combining healthcare with AI-based financial technology is one of the fastest-growing industries. This fits perfectly with MedBillionaires™’ mission.
These partnerships aim to make advanced healthcare tech available to more people, not just big companies. Each collaboration helps the company grow in a sustainable way, while ensuring transparency and strong operations.
The Future of MedBillionaires and Healthcare Innovation
The combination of AI and FinTech is changing the way healthcare is delivered, and MedBillionaires is at the forefront of this revolution. As technology continues to advance, we can expect even more innovations in areas such as machine learning, predictive healthcare, and financial automation.
In the near future, AI-powered systems may be able to predict disease outbreaks, personalize treatments with even greater accuracy, and enhance the overall patient experience. Meanwhile, FinTech will continue to drive down costs, making healthcare accessible to a larger portion of the population.
MedBillionaires is also exploring ways to integrate more advanced payment systems, such as cryptocurrencies, and further expand its AI-driven offerings to cover a broader range of healthcare needs. The company’s vision is to create a future where healthcare is not only smarter but also more accessible, transparent, and affordable.
The Road Ahead
As MedBillionaires™ grows, it stays focused on changing how healthcare operates and is financed. By combining AI technology, Med-FinTech systems, and the Pre-Public Company™ framework, the company makes sure its platform is flexible, scalable, and ready for the future.
MedBillionaires™ is not just keeping up with healthcare’s future it’s creating it. With a strong vision, solid leadership, and a focus on technology, the company aims to change the way people experience healthcare innovation.
-
Business2 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business2 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business2 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health2 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports2 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom































