health
The Future of Diabetes Treatment

Care
Right Family Dentist in Cypress, TX: A Comprehensive Guide

Choosing a dentist for your family is a significant decision, more personal than many realize. It goes beyond merely booking dental cleanings; it’s about entrusting someone with your comfort, health, and often your confidence. In a close-knit community like Cypress, TX, that trust holds even greater importance. Families seek care that feels familiar, consistent, and genuinely focused on their long-term well-being.

The Importance of Oral Health
Oral health impacts daily life in countless ways that often go unnoticed. It shapes how you eat, how you speak, and influences your self-esteem in social situations. When dental care is rushed or inconsistent, small issues can escalate into painful problems. Many families in Cypress prioritize proactive dental care, aiming for a preventive approach rather than a reactive one.
For those seeking a reliable practice that can accommodate various ages and stages, Cypress family dental care offers a unique solution. This comprehensive approach fosters continuity. Instead of hopping between different offices, families can develop relationships with a team that understands their specific history and priorities. This familiarity leads to informed decisions, fewer emergency situations, and a more streamlined experience.
What Comprehensive Dental Care Looks Like
Comprehensive dentistry is rooted in the understanding that no two patients are identical. This approach integrates prevention, education, treatment, and long-term planning into a cohesive system. Instead of waiting for discomfort to arise, dentists prioritize maintaining health and preventing future issues.
Preventive care lays the foundation for everything. Regular check-ups and cleanings facilitate early detection of problems like decay and gum disease. These visits also allow patients the opportunity to ask questions and learn better habits, as minor adjustments to daily routines can result in a lifetime of dental health.
When therapeutic intervention is necessary, restorative dentistry comes into play. Treatments such as fillings, crowns, and root canal therapy restore lost tooth structures. Many patients find that modern procedures are far more routine and less painful than they had anticipated.
Cosmetic care plays its part, as well. Treatments like whitening, bonding, and veneers can revitalize smiles and boost self-confidence. However, they also contribute to long-term oral health by improving the structure and cleanliness of teeth.
While some patients might require orthodontic intervention for issues related to teeth spacing or bite, the coordination of these services within a single practice offers considerable benefits. This integration helps families manage their dental care more efficiently.
Why Family Dentistry Matters in Cypress, TX
Cypress continues to grow, attracting families who value strong schools, safe neighborhoods, and reliable healthcare. This growth generates a demand for consistent dental providers who focus on long-term care rather than quick fixes.
Family dentistry simplifies life for parents. Appointments can be easily coordinated, medical records remain consolidated, and overall care feels more cohesive. Parents appreciate not needing to repeat their children’s medical histories at every visit. Children, in turn, benefit from regularly seeing the same friendly faces.
For adults, this continuity translates to better health outcomes. A dentist familiar with your past treatments can detect changes early and tailor care to fit your individual needs. This long-term perspective often prevents the need for more extensive interventions down the line.
Just as crucial is the comfort that comes with familiarity. Entering an office where the staff recognizes you increases the likelihood of a positive experience, making routine visits manageable rather than anxiety-inducing.
Supporting Children and Creating Healthy Foundations
Early dental treatment sets the stage for a child’s lifelong relationship with oral health. When children feel comfortable in the dental office, they are more likely to maintain good habits as adults. Regular check-ups allow dentists to monitor tooth development and jaw growth, identifying issues related to crowding or bites before they become significant problems.
Preventive measures such as sealants and fluoride treatments provide added layers of protection. Sealants guard molars against decay, while fluoride strengthens enamel. These small steps can prevent years of dental issues down the road.
Creating a welcoming atmosphere is crucial for children’s visits. Trust is established when kids feel respected and heard, making them active participants in their own care rather than passive recipients of treatment.
Navigating Teen Years and Changing Dental Needs
The teenage years can present unique challenges for oral health. Hormonal changes may impact gum health, and busy lifestyles can lead to disrupted brushing routines. This stage is also when many families start considering orthodontic options.
Orthodontic care is not just about aesthetics; it offers functional benefits, too. Straightening teeth can improve bite function and make daily cleaning simpler, boosting overall confidence. Dentists collaborate with families to explore the best options, whether that’s traditional braces or clear aligners while monitoring wisdom tooth development.
Teen dental care emphasizes more than just appearance; it encourages personal responsibility and forms healthy habits that will last a lifetime.
Adult Dental Care: Maintenance and Restoration
For adults, maintenance and restorative procedures become the primary focus. Balancing work, family, and personal life can make it easy to postpone dental appointments, yet neglecting minor issues often leads to more significant problems.
Routine check-ups enable the early detection of decay and gum disease, both of which have significant implications for overall health. Neglected gum health can lead to tooth loss and has been linked to other serious health conditions.
Restorative procedures, such as crowns, implants, and bridges, not only restore functionality but also enhance comfort. Many adults find that enhancing their dental work can significantly improve their quality of life.
Cosmetic treatments like bonding and whitening can also boost confidence, creating positive effects in both personal and professional spheres.
Dental Care for Seniors: Emphasizing Comfort and Function
As individuals age, their oral health needs become more complex. Factors like enamel wear, gum recession, and changes in saliva production require age-specific care strategies.
Dentists monitor for issues such as dry mouth, gum disease, and oral cancers while maintaining existing restorations to ensure comfort and proper function. These considerations directly influence nutrition, speech, and overall wellness.
Education and guidance remain vital for seniors. Dentists provide advice on hydration, diet, and at-home care routines that support oral health, making many age-related challenges manageable.
Staying with a trusted dental team can offer peace of mind for seniors. Long-term relationships foster trust, reducing anxiety about ongoing care.
Practical Ways to Maintain Your Family’s Oral Health
Building Consistent Routines: Encourage brushing twice daily with fluoride toothpaste and daily flossing. Consistency often trumps perfection.
Scheduling Regular Visits: Most families benefit from biannual check-ups, allowing dentists to conduct thorough cleanings and catch issues before they escalate.
Making Healthy Food Choices: Reducing sugary snacks and acidic beverages can lower the risk of cavities. Prioritizing water, fresh produce, and calcium-rich foods strengthens teeth and gums.
Protecting Teeth During Activities: Use mouth guards during sports and avoid using teeth as tools to prevent damage.
Responding to Early Signs: Sensitivity, bleeding gums, or lingering discomfort shouldn’t be ignored. Addressing these concerns early typically leads to simpler treatments.
The Importance of Choosing Local Dental Care
Local practices provide personalized services that larger operations may lack. Families in Cypress appreciate providers who understand their routines and community dynamics, fostering relationships based on trust.
When searching for dental care, many families prioritize local providers. This relationship encourages proactive care and long-term commitments, resulting in fewer last-minute visits.
Patients also benefit from personalized communication. A local practice remembers preferences and follows up with care, establishing a human connection that enhances the overall experience.
Making Informed Orthodontic Choices
Deciding on orthodontic treatment can be daunting, but understanding the process helps set realistic expectations. Reviewing before-and-after pictures offers patients clarity about potential outcomes.
Dentists clarify timelines and daily care requirements, emphasizing the significance of aligned teeth for overall oral health. By prioritizing education over pressure, dental professionals empower families to make informed decisions.
A Long-term Approach to Family Dental Health
Achieving dental wellness requires more than one visit; it necessitates years of thoughtful care and open discussions. Families that embrace this mindset experience fewer emergencies and greater confidence in their dental health.
In Cypress, where community and quality of life are paramount, selecting a dental provider becomes an investment in the family’s future. Family dentistry aims not only to keep teeth healthy but also to promote well-being through preventive care, modern solutions, and effective communication.
Frequently Asked Questions
How often should families visit the dentist?
Typically, every six months, but your dentist may recommend a different schedule based on individual needs.
When should a child first see a dentist?
At age one or when the first tooth appears.
Can adults receive orthodontic treatment?
Absolutely; many adults benefit from braces or clear aligners.
What if a family member is anxious about visiting the dentist?
A patient-centered dental team prioritizes comfort and explains procedures in detail to help ease fears.
What are the benefits of local dental care?
Local practices often offer personalized services, easier follow-ups, and build trust within the community.
Care
How Technology is Transforming Hospital care for Patients

Are you struggling with an outdated hospital care system? Do you wish to be treated immediately? This is achieved through technological advancement within our healthcare to simplify processes and help patients.
In this blog we will discuss how technology is changing the entire patient journey.
For example, the best gynecologist in Multan is already integrating these advancements into their healthcare system. In the digital age, no sector has been left unconverted with technology for so long as healthcare.
Therefore, we can witness these advancements in the form of telemedicine and robotic surgery in our healthcare system. Every new development is making hospitals more productive and patient-centered, with healthy recovery of patients.
As patients, we should have awareness about advanced tools and technology as a way to help our healthcare experts and to enhance our ordinary reports.
The Role of Telemedicine in Revolutionizing Patient Access
Telemedicine is also one of the greatest innovations in hospital care over the past few years. This way, patients can remotely meet with doctors and won’t need as many in-office visits.
For example, you no longer have to go visit healthcare providers; instead, now they can reach out to you at your home, which will save time for people and make health services easily accessible.
However, in remote areas routine visits, follow-up, or first consults, telemedicine is closing the gap between patient and doctor.
Artificial Intelligence (AI) and Machine Learning in Diagnostics
Diseases are not diagnosed like they once were. Now artificial intelligence algorithms exist that can analyze medical images, predict a patient’s likelihood to develop a particular disease, or even offer types of treatments to try.
AI systems help hospitals to treat and diagnose conditions more effectively and quickly. AI can be applied in radiology to spot abnormalities on X-rays and MRIs, assisting doctors in making quicker and more informed decisions.
It’s not just about early detection, when AI is used in treating patients at hospitals, it improves the standard of care a patient has access to.
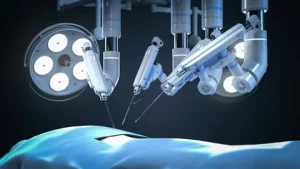
Robotic Surgery: Precision and Recovery
Another technical tool that is revolutionizing the hospital system is robotic surgery. This development enables surgeons to manage complex surgeries with higher precision.
However, if we compare traditional approaches, robotic surgery allows a greater range of motion and precision, resulting in smaller incisions, less blood loss, and faster recovery for the patient.
Doctors can perform minimally invasive surgeries with less pain and quicker recovery for patients. People choose only those healthcare centers where they have access to these ground-breaking technologies, and are guaranteed high-quality care.
Patient Monitoring: Real-time Care at Its Best
Thanks to wearable health devices and remote monitoring resources, hospitals can track the vital signs of patients in real time. That allows doctors and nurses to act immediately if they see any change in a patient’s condition.
ICU patients or other patients who need to be observed are now possible to monitor from a distance, yet with immediate assistance response all day.
For example, the best hospital in Multan is using new technological advancements to increase patient safety and eliminate clinical error.
Electronic Health Records (EHR): Streamlining Patient Data
The adoption of electronic health records (EHR) is one of the biggest things to ever happen to hospital care. EHR systems allow you to access and store data more quickly than ever.
This eliminates the need for paper-based documentation and minimizes issues caused by documentation errors. It ensures your security, only you and those people in your care circle are able to access your information online.
Virtual Reality (VR) for Pain Management and Surgical Training
Virtual reality is a relatively new way for hospitals to address pain management and medical training, yet it’s producing strong results.
For pain relief and pain management, VR provides non-invasive and drug-free solutions to keep patients comfortable by reducing pain and anxiety during medical procedures.
Doctors can improve their skills and can practice complex procedures by seeing how they’d perform in a virtual environment before applying them in a real patient’s treatments.
The Future of Hospital Care
Looking ahead, technology in healthcare will be even bigger. From 3D printing personalized prosthetics and virtual reality models for healthcare provider training to blockchain for managing patient data securely, we have exciting times ahead.
Hospitals will transform into increasingly modern, high-tech facilities in which quality of care is enhanced through creativity. AI-powered systems are serving patients with more care and efficiency.
Final Thoughts
So, we can say that technology is transforming the hospital landscape in deep ways. It smoothens the administrative tasks and assists healthcare specialists to improve hospital services.
Whether it is telemedicine connecting patients with specialists or robotic surgery that improves the outcome of procedures, technology is both improving the standard of healthcare and making delivery to our patients more accessible and efficient.
Thanks to these breakthroughs, hospitals can become more patient-focused, meaning we all stand to benefit from better experiences in healthcare.
Care
The Essential Benefits of Shilajit for Men’s Health

Men today face multiple health challenges due to busy schedules, work pressure, lack of physical activity, and poor lifestyle habits. Over time, these factors can lead to low energy levels, reduced stamina, hormonal imbalance, stress, and overall weakness. To counter these issues naturally, many men are turning towards traditional Ayurvedic remedies—one of the most powerful being Shilajit.
Shilajit has been used in Ayurveda for centuries and is known for its rejuvenating and strengthening properties. This blog explains the key Shilajit benefits for men, how it works, and why it is becoming an essential supplement for modern male health.

What Is Shilajit?
Shilajit is a natural substance formed over hundreds of years from the gradual decomposition of plants and minerals found in high-altitude mountain regions, especially the Himalayas. It appears as a dark, sticky resin and is rich in fulvic acid, humic substances, and essential trace minerals.
In Ayurveda, Shilajit is classified as a Rasayana, meaning a rejuvenator that helps improve strength, longevity, and overall health. When purified and consumed correctly, Shilajit supports multiple body systems and is especially beneficial for men.
1. Boosts Energy Levels and Reduces Fatigue
One of the most common reasons men take Shilajit is to fight constant tiredness and low energy. Modern lifestyles often leave men feeling drained due to stress, long working hours, and lack of rest.
Shilajit helps improve energy production at the cellular level by supporting mitochondrial function. This allows the body to produce energy more efficiently, resulting in reduced fatigue and improved physical performance.
Regular consumption may help men feel more active, energetic, and less exhausted throughout the day.
2. Supports Healthy Testosterone Levels
Testosterone is a vital hormone for men. It plays a major role in muscle mass, strength, stamina, mood, and sexual health. As men age, testosterone levels naturally decline, which can lead to weakness, low libido, and reduced motivation.
One of the key Shilajit benefits for men is its ability to support natural testosterone production. When taken consistently, purified Shilajit may help maintain healthy hormone levels without relying on synthetic supplements.
This makes Shilajit particularly useful for men above the age of 30 who want to support hormonal balance naturally.
3. Improves Stamina and Physical Endurance
Whether it is daily work, exercise, or sports, stamina plays a crucial role in a man’s physical performance. Shilajit helps improve oxygen utilisation and nutrient absorption, which supports better endurance and reduced physical exhaustion.
Men who consume Shilajit regularly often report improved stamina, better workout performance, and quicker recovery after physical activity. This makes it a popular choice among fitness enthusiasts and men with physically demanding lifestyles.
4. Enhances Sexual Health and Libido
Sexual health is closely linked to confidence and emotional well-being in men. Stress, poor diet, and hormonal imbalance can negatively affect libido and sexual performance over time.
Shilajit has traditionally been used as a natural aphrodisiac in Ayurveda. It helps improve blood circulation, supports testosterone levels, and enhances overall reproductive health.
Some of the key Shilajit benefits for men in terms of sexual wellness include improved libido, better stamina, and enhanced performance. With regular use, many men experience improved confidence and satisfaction.
5. Supports Muscle Growth and Strength
Men aiming to build muscle or maintain strength can benefit significantly from Shilajit. It helps the body absorb nutrients more effectively and supports protein synthesis, which is essential for muscle development.
Shilajit also helps reduce muscle soreness and fatigue after intense physical activity. When combined with proper nutrition and regular exercise, it can support muscle strength and long-term fitness goals.
6. Improves Mental Focus and Reduces Stress
Mental stress and lack of focus are common problems among working men today. Constant pressure, long screen time, and poor sleep can affect cognitive function and mental clarity.
Shilajit contains fulvic acid, which acts as a natural antioxidant and helps reduce oxidative stress in the brain. Regular intake may help improve concentration, memory, and mental stamina.
Men who use Shilajit often report better focus at work, reduced stress levels, and improved overall mood.
7. Strengthens Immunity and Overall Health
A strong immune system is essential for staying healthy and active. Shilajit contains essential minerals and bioactive compounds that help strengthen the body’s natural defence system.
For men who frequently feel weak or fall sick often, Shilajit can help improve immunity and overall resistance. It also supports better nutrient absorption, ensuring the body gets maximum benefit from food and supplements.
8. Supports Heart Health and Blood Circulation
Heart health becomes increasingly important as men age. Shilajit helps support healthy blood circulation and may help maintain balanced cholesterol levels when used as part of a healthy lifestyle.
Improved blood flow not only supports heart health but also contributes to better stamina, energy levels, and sexual wellness in men.
How to Take Shilajit for Best Results
For most men, the recommended dosage is around 300–500 mg of purified Shilajit per day. It is best consumed with warm water or milk, preferably in the morning on an empty stomach, as this is considered the best time to take shilajit for maximum absorption and effectiveness.
Consistency is important. Most benefits become noticeable after a few weeks of regular use.
Important Things to Keep in Mind
- Always choose purified and lab-tested Shilajit
- Avoid raw or unprocessed forms
-
Individuals with preexisting health issues should seek advice from a medical expert prior to use
Conclusion: Is Shilajit Good for Men?
Shilajit offers multiple benefits for men, including improved energy, stamina, testosterone support, sexual health, mental focus, and overall well-being. In today’s demanding lifestyle, this ancient Ayurvedic remedy provides a natural way to restore balance and vitality.
When taken regularly and responsibly, Shilajit can be a valuable addition to a man’s daily health routine.
-
Business3 years ago
Cybersecurity Consulting Company SequelNet Provides Critical IT Support Services to Medical Billing Firm, Medical Optimum
-
Business3 years ago
Team Communication Software Transforms Operations at Finance Innovate
-
Business3 years ago
Project Management Tool Transforms Long Island Business
-
Business2 years ago
How Alleviate Poverty Utilized IPPBX’s All-in-One Solution to Transform Lives in New York City
-
health3 years ago
Breast Cancer: The Imperative Role of Mammograms in Screening and Early Detection
-
Sports3 years ago
Unstoppable Collaboration: D.C.’s Citi Open and Silicon Valley Classic Unite to Propel Women’s Tennis to New Heights
-
Art /Entertainment3 years ago
Embracing Renewal: Sizdabedar Celebrations Unite Iranians in New York’s Eisenhower Park
-
Finance3 years ago
The Benefits of Starting a Side Hustle for Financial Freedom